DBP3:UCLA
Back to NA-MIC DBPs | NA-MIC Cores
Contents
- 1 Introduction
- 2 Project Goals and Specific Aims
- 3 Methods
- 4 Current Tasks
- 5 Results
- 6 Outreach
- 6.1 Outreach Events
- 6.1.1 UCLA Neurology Science Day (January 2011)
- 6.1.2 TBI DBP Meeting at NA-MIC AHM (January 2011)
- 6.1.3 TBI DBP Conference Call with Utah Team (September 9, 2011)
- 6.1.4 NA-MIC Conference Call (October 27, 2011)
- 6.1.5 TBI DBP Conference Call (November 10, 2011)
- 6.1.6 NA-MIC Conference Call (November 16, 2011)
- 6.1.7 UCLA visit by Dr. Guido Gerig from Univ. of Utah (May 22, 2012)
- 6.1.8 NA-MIC All Hands Meeting (January 2013)
- 6.1.9 UCLA-HMS-Utah Collaborative Meeting (April 2013)
- 6.1.10 USC Workshop on 3D Slicer for Brain research (February 2013)
- 6.1 Outreach Events
- 7 Investigators
- 8 Awards, Honors and Accomplishments
- 9 Publications
- 10 Press Releases
- 11 Links
Introduction
What is traumatic brain injury?
Traumatic brain injury, often referred to as "TBI", is most often an acute event that results in severe damage to portions of the brain. TBI results when the head suddenly and violently hits an object, or when an object pierces the skull and enters brain tissue. Symptoms of can be mild, moderate, or severe, depending on the extent of the damage to the brain. Common disabilities include cognitive deficits, sensory processing, communication, and behavior or mental health. Severe TBI may result in stupor where an individual can be aroused briefly by a strong stimulus (e.g. sharp pain); coma, where an individual is totally unconscious, unresponsive, unaware, and un-arousable; vegetative state, where an individual is unconscious and unaware of his or her surroundings, but continues to have a sleep-wake cycle and periods of alertness; and a persistent vegetative state, where an individual remains unresponsive for more than a month.
According to the CDC (United States Centers for Disease Control and Prevention), there are approximately 1.7 million people in the U.S. who suffer from a traumatic brain injury each year. 50,000 people die from TBI each year and 85,000 people suffer long term disabilities. In the U.S., more than 5.3 million people live with disabilities caused by TBI. Patients admitted to a hospital for TBI are included in this count, while those treated in an emergency room or doctor's office are not counted. The causes of TBI are diverse. The top three causes are: car accident, firearms and falls. Firearm injuries are often fatal: 9 out of 10 people die from such injuries. Young adults and the elderly are the age groups at highest risk for TBI. Along with a traumatic brain injury, persons are also susceptible to spinal cord injuries which is another type of traumatic injury that can result out of vehicle crashes, firearms and falls. Prevention of TBI is the best approach since there is no cure or way to reverse brain damage of this kind.
Mechanisms of TBI
Understanding the various mechanisms of TBI can be helpful for the development of robust and reliable computational algorithms for neuroimage data processing. These mechanisms are the highest causes of brain injury: Open head Injury, Closed Head Injury, Deceleration Injuries, Chemical/Toxic, Hypoxia, Tumors, Infections and Stroke.
1. Open Head Injury
* Results from bullet wounds, etc. * Largely focal damage * Penetration of the skull * Effects can be just as serious as closed brain injury
2. Closed Head Injury
* Resulting from a slip and fall, motor vehicle crashes, etc. * Focal damage and diffuse damage to axons * Effects tend to be broad (diffuse) * No penetration to the skull
3. Deceleration Injuries (Diffuse Axonal Injury) The skull is hard and inflexible while the brain is soft with the consistency of gelatin. The brain is encased inside the skull. During the movement of the skull through space (acceleration) and the rapid discontinuation of this action when the skull meets a stationary object (deceleration) causes the brain to move inside the skull. The brain moves at a different rate than the skull because it is soft. Different parts of the brain move at different speeds because of their relative lightness or heaviness. The differential movement of the skull and the brain when the head is struck results in direct brain injury, due to diffuse axonal shearing, contusion and brain swelling.
Diffuse axonal shearing: when the brain is slammed back and forth inside the skull it is alternately compressed and stretched because of the gelatinous consistency. The long, fragile axons of the neurons (single nerve cells in the brain and spinal cord) are also compressed and stretched. If the impact is strong enough, axons can be stretched until they are torn. This is called axonal shearing. When this happens, the neuron dies. After a severe brain injury, there is massive axonal shearing and neuron death.
4. Chemical/Toxic
* Also known as metabolic disorders * This occurs when harmful chemicals damage the neurons * Chemicals and toxins, e.g. insecticides, solvents, carbon monoxide poisoning, lead poisoning, etc.
5. Hypoxia (Lack of Oxygen)
* If the blood flow is depleted of oxygen, then irreversible brain injury can occur from anoxia (no oxygen) or hypoxia (reduced oxygen) * This condition may be caused by heart attacks, respiratory failure, drops in blood pressure and a low oxygen environment * This type of brain injury can result in severe cognitive and memory deficits
6. Tumors
* Tumors caused by cancer can grow on or over the brain * Tumors can cause brain injury by invading the spaces of the brain and causing direct damage * Damage can also result from pressure effects around an enlarged tumor * Surgical procedures to remove the tumor may also contribute to brain injury
7. Infections
* The brain and surrounding membranes are very prone to infections if the special blood-brain protective system is breached * Viruses and bacteria can cause serious and life-threatening diseases of the brain (encephalitis) and meninges (meningitis)
8. Stroke
* If blood flow is blocked through a cerebral vascular accident (stroke), cell death in the area deprived of blood will result * If there is bleeding in or over the brain (hemorrhage or hematoma) because of a tear in an artery or vein, loss of blood flow and injury to the brain tissue by the blood will also result in brain damage
In this DBP, we will be primarily concentrating on #'s 1, 2, and 3.
Neurological Concomitants of TBI
Following TBI, a cascade of neuroanatomical alterations initiate, with diffuse alterations in cortical structure peripheral to the point of injury but also distributed throughout the brain. Notably, there is ventricular enlargement and cortical thickness changes remote from the site of the TBI. White matter connectivity can be significantly altered with greatly reduced efficiency of signal transduction over affected pathways or complete cessation of inter-regional communication due to axonal damage. This can have profound effects on speech, motor, and cognitive processes. The extent of change is putatively related to the severity of TBI, location, subject age, and post-injury treatment, among other factors.
Challenges of TBI Neuroimaging
On anatomical MRI scans, TBI-related insults can appear as hyper-intensities, varying in magnitude and extent the degree to which tends to correlate with clinical symptoms. Additionally, in severe TBI, sections of skull, fractured during the injury or removed during surgical intervention, may not form a contiguous boundary enabling efficient digital removal of bone and other non-brain tissues, complicating tissue segmentation, regional parcellation, the measurement of ventricular size, cortical thickness, and other metrics. Computational algorithms require refinement to include constraints to account for TBI related signal alterations in anatomical scans; e.g. users may have to manually indicate regions encompassing the site of injury on the scans to guide local processing around the site and to reduce the weight of these regions on other, non-affected brain areas. Alternatively, probabilistic classifiers may need to include an extra classification for voxels whose tissue properties have been altered by TBI. This is particularly the case in diffusion weighted imaging (DWI) where the presence of TBI-related alterations in signal may reflect specific damage to white matter proximal to the lesion as well as long reaching effects along tracts to peripherally connected regions of cortex.
Project Goals and Specific Aims
Project Goals
An increasingly relevant means for the neurological assessment of traumatic brain injury (TBI) is with in vivo neuroimaging. However, standard automated image analysis methods are not robust with respect to the TBI-related changes in image contrast, changes in brain shape, cranial fractures, white matter fiber alterations, and other signatures of head injury. Multimodal quantification of brain insults and associating these with clinical and outcome metrics is a particular challenge. The emphasis in this DBP is placed on the feasibility of subject-specific analysis, as opposed to population-based averaging, to examine the influence of TBI on time-dependent alteration of gray and white matter integrity with accompanying change in clinical outcome variables to be used in subsequent TBI assessment. This DBP [1] seeks to:
1. Develop end-to-end processing approaches using the NA-MIC Kit to investigate alterations in cortical thickness, and subsequent ventricular and white matter changes in patients with TBI and in age-matched controls. Image processing will include segmentation of lesions, hemorrhage, edema, and other pathology relevant to TBI. Longitudinal changes will be assessed by registration and joint segmentation of baseline and follow-up data.
2. Develop robust workflows for diffusion weighted imaging (e.g. DTI, HARDI) datasets from TBI patients, by using the NA-MIC Kit and Slicer to obtain reliable and robust metrics of white matter pathology and of white matter changes due to therapy and/or recovery.
3. Using the NA-MIC Kit, cross-correlate multimodal metrics of cortical thickness, complexity, ventricular volume, and lesions from structural imaging and white matter fiber integrity from diffusion tensor imaging, with clinical outcome variables, i.e., time since injury, age, gender and other potential factors predictive of recovery.
Specific Aims
In this NA-MIC DBP, we seek to develop the means for guided and semi-automatic TBI analysis and quantification with a view toward assessing clinical improvement under the following Specific Aims:
Aim 1
How can multimodal assessment of altered brain anatomy speak directly to questions of brain plasticity and to secondary neuroanatomical effects of TBI?
We will develop end-to-end processing approaches using the NA-MIC Kit to investigate alterations in cortical thickness, subsequent ventricular, and white matter changes in patients with TBI and in age-matched controls.
Aim 2
Can multimodal workflows be developed to guide clinicians in the analysis and display of white matter fiber tract pathology that frequently accompanies brain insult?
In diffusion weighted imaging (e.g. DTI, HARDI) datasets from TBI patients, we will develop robust workflows using the NA-MIC Kit and Slicer to obtain reliable and robust metrics of white matter pathology.
Aim 3
How can multimodal metrics of TBI grey and white matter pathology be utilized to inform and guide clinical assessment?
Under this DBP, using sophisticated NA-MIC tools, we will develop end-to-end processing solutions by which to examine TBI neuroimaging data. The NA-MIC Kit encompasses a collection of tools for automated or semi-automated processing of medical imaging data. Notable is the Insight Toolkit (http://www.itk.org) for use in brain registration and segmentation via the 3D Slicer (http://www.slicer.org) software platform. These software tools may be linked to form data processing workflows that can process data via end-to-end solutions that may be shared with others, posted on websites, and used in training materials. They form an excellent platform for user-guided, patient-specific analysis, however, require additional development to inform the program about regions where TBI-related signal changes may necessitate alteration of model parameters or search volumes. Using the NA-MIC Kit, multimodal metrics of cortical thickness, complexity, and ventricular-volume from structural imaging and white matter fiber integrity from diffusion tensor imaging will be cross-correlated with clinical outcome variables, time since injury, age, gender and other potential factors predictive of recovery. We will emphasize the feasibility of subject-specific analysis, as opposed to population-based averaging, to examine the influence of TBI on time-dependent alteration of gray and white matter integrity with accompanying change in clinical outcome variables to be used in subsequent TBI assessment.
This DBP directly pertains to stated scientific and funding objectives of the NIBIB and other NIH institutes conducting (e.g. NINDS) and supporting (e.g. NCRR) research on the mechanisms underlying CNS injury; to develop intervention strategies to limit the primary and secondary brain damage occurring within days of a TBI; and to devise therapies to treat TBI and help in long-term recovery of function. DBP results will have important implications for national health policy concerning TBI awareness, treatment and brain plasticity. Thus, this DBP is directly in-line with the NIH mission for greater assessment of neurological insults and factors that predict long-term outcomes in individual patients.
Methods
Software and Analysis Protocol
We will specifically adopt the NA-MIC kit open source software platform consisting of Slicer, tools and toolkits such as VTK and ITK, and software engineering methodologies for multiplatform implementation. Using ITK, data will be intensity normalized and bias-field corrected; tissue types will be segmented interactively to assist probabilistic classification; cortical thickness will be determined along the entire cortical sheet as the linear distance between the outer edge of the cortical surface and the grey-white matter boundary. Ventricular size will be determined by a space filling algorithm, while shape will be characterized using LONI tools for shape decomposition and quantitative description. DWI processing routines will be developed to better account for TBI-related changes in diffusion metrics. Results from multimodal analyses will be visualized using VTK, Slicer, and other suitable platforms.
Anatomical Data
To rigorously assess workflows using the NA-MIC Kit, we will examine neuroimaging data obtained from TBI patients. MRI volumes from 202 subjects will be drawn from the LONI Image Data Archive (IDA), a comprehensive neuroimaging data archive comprised of a number of funded projects. Samples will include patients who have suffered from TBI (N=160; 22F:138M) and age-matched normal controls (N=42; 13F:29M). Mean±sd ages for males is 33.8±9.2 and for females is 33.6±9.9. T1-weighted whole brain MPRAGE volumes, T2, and, in subjects with available data sets, diffusion weighted imaging (DTI/HARDI) collected at 1.5 and 3.0T will be utilized. Additional data include a variety of MR imaging modalities and NA-MIC workflows will be crafted to accommodate them.
Expected Results
Multimodal results will be obtained using Slicer software tools, specifically developed under NA-MIC using ITK, VTK, for the analysis of neurological concomitants of TBI. Metrics will be extracted and imported into purpose built software for univariate and multivariate modeling to provide additional insights to that of previous work on the role of neuroanatomical changes occurring in TBI on outcome variables predicting degree of change and/or recovery. Several primary hypotheses using individual and repeated imaging include:
1. Cerebral atrophy (regional and global) occurs at a faster rate in diffuse vs. focal TBI;
2. Rates are dependent upon initial injury severity
3. Ongoing or progressive change continues up to 1 yr post-TBI
4. Secondary insults increase the rate and extent of the initial TBI
We will also examine age-at-lesion effects, since these factors are likely to impact on measures of the degree of loss of developmental and life-span neuroplasticity believed to follow TBI. Using DWI data, we will assess the effects of TBI on mean diffusivity, fractional anisotropy, and their potential as clinical outcome correlates. Complete multimodal data processing solutions using the NA-MIC Kit and associated tools will be made openly available, with accompanying training materials via the NA-MIC web site, and comply with the NA-MIC open-source policies.
Clinical Utility
The emphasis from the NA-MIC KIT workflows developed under this program will be on the application of the NA-MIC tools to TBI clinical practice and patient monitoring. With knowledge of general location, extent, and degree of change, such metrics can be associated with clinical measures and used to suggest viable treatment options for a subject against patterns typical of TBI patients.
Current Tasks
Considerable interactions presently exist between the NA-MIC project and LONI, resulting in numerous peer-reviewed publications. This shows the suitability of these teams to work jointly under this proposed project. Computational outcomes from this DBP will also directly contribute to other NA-MIC DBPs involving
1. mapping head and neck radiation therapy
2. tracking MRI brain changes in Huntington’s Disease
3. segmenting cardiac MR atrial wall ablations in arrhythmia patients.
USC investigators will interact directly with NA-MIC Core 1 and 2 PIs in developing new and refining existing processing algorithms for addressing the issues inherent to neuroimaging data from TBI patients (YR1). DBP activities at USC will occur in consultation with the Primary Technical NA-MIC DBP Contact and the Algorithm and Engineering Contact. Once completed and rigorously validated these workflows will
1. be applied to the TBI patient data described above (YR1-2)
2. be made available for open dissemination via the NA-MIC website (YR3)
3. form the basis for training and educational materials for NA-MIC investigators and the TBI community (YR3)
Results will be featured in presentations at scientific conferences, organized training events/workshops, etc., as a way to disseminate tool capabilities and, where possible, tutorials on how to use the NA-MIC technology for other TBI-related projects. We will attend each NA-MIC All-Hands-Meeting to discuss the DBP with NA-MIC PIs, report on developments, and progress. NA-MIC will benefit from this DBP by exposure to a unique community that often possesses multisite neuroimaging clinical trials data.
Case Analysis Goals
- Multimodal registration within and between scan sessions separated by ~6 months
- Computation of neuroanatomical measures of change per unit time in each case
- Visualization of 3D models and their degree of change
- Quantification of alterations in ventricle and WM/GM volume, surface, cortical thickness, and other morphological metrics at time 1 and time 2
- Ability to quantify changes in diffusion local to the lesions as well as overall mean FA and fiber patterns between scan sessions
- Generation of a clinical report for each TBI patient. The clinician should have the ability to store such a report and use it in conjunction with their neurological assessments to gain insight about the case. It would be nice if that report could be generated not only in printer-friendly format but also in XML (or similar format) so that it can be read without much trouble into Matlab, R, or other secondary analysis frameworks or databases.
- Semi-automatic segmentation. Certain aspects of image segmentation segmentation may need to be user-guided (e.g. to conditionalize segmentation given the presence of a lesion), though in a way that is easy for clinicians to use. The user might point and click on an area exhibiting a bleed, or some other type of hypo-/hyperintesity. A boundary contour could then be found around that area, and the segmentation model would then be weighted by the presence of that area as some unique tissue type.
- Creation of population-based atlases from multiple TBI subjects or at least reference to standardized coordinate systems
Software Requests
- The UCLA team would like to have Windows compilations of (1) the Longitudinal Lesion Comparison and (2) the Lesion Segmentation Applications Modules.
Specific Tasks In Progress
Specific tasks include the following, in reverse chronological order:
- There is some interest in a macro capability to record selections for later playback
- Full brain fiber tractography
- NIFTI 4D file read/write, external gradient information importation, and a gradient table editor for DTI
- Better interoperability between LPS/RAS file organization in Slicer vs. vTK
- Ability to set direction cosines directly in Slicer volumes module
- Timed autosave functionality of scene files and other filetypes fundamental to Slicer (saved for several time steps)
- Welcome screen should be a pop-up window in the middle of screen that could be disabled
- Integration of volume render with slice displays (rendering set aside as an option)
- Import tools for DTIStudio and TrackVis tractography files
- Creating 3D ROIs using the edge detection routine
- Use of customizable toolbars for commonly used operations/features/modules/workflows/etc
- Volumes shouldn’t be loaded differently from “other data”
- Screen shot functionality shouldn’t force a re-render
- Being able to record video sequences (at least we couldn’t readily find this capability)
- NIFTI fMRI processing capability (3D+time)
Completed
- 2010-Dec-20. ABC module has been successfully compiled for Windows and tested (use Slicer nightly build for best results). Our thanks to Marcel and to the Utah team!
- 2011-Jan. TubeTK implementation of slicing organ registration made available in Slicer4 at AHM in Salt Lake City
- 2011-Oct. Geometric Metamorphosis presentation at MICCAI 2011
- 2011-Oct. Sliding organ registration presented at Abdominal Imaging workshop at MICCAI 2011
- 2012-Jan. CalaTK implementation of geometric metamorphosis for registration in the presence of lesion infiltration/recession released
- 2012-Oct. Sliding organ journal article submitted to IEEE Transactions on Medical Imaging
Results
Sample Slicer Results
The following PDF contains a presentation prepared by Dr. Guido Gerig which showcases some example results on the above TBI data sets obtained using existing and newly developed Slicer processing modules.
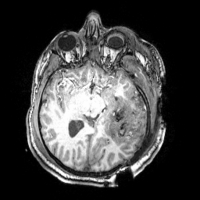
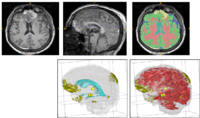
TBI Results at UCLA
The ABC module in 3D Slicer has been applied to segment the anatomic MR volumes for Patients 1-3 in the Sample Data Sets section. In the adjacent figures, sample images of the segmentations for Patient 3 (both acute baseline and follow-up) are shown. In the first image, the WM and GM segmentations are shown for the acute baseline and follow up scans of Patient 3. We have found that, for this TBI patient, the ABC segmentation is superior to that of the EMSegmenter Module and we are excited about the ability of ABC to capture the neuroanatomical outliers of these challenging data. Many of the items of concern that remain concerning the quality of the segmentation might be addressed using suitable modifications of input parameters to ABC. For example, there seems to be some inconsistency between scans in the reconstructed gyrification of the cortex and extent of the GM/WM interface (see arrows, first and third columns). We are looking forward to learning more about the effective use of ABC to avoid these problems.
From the second figure it can be inferred that, in the case of the acute baseline scan, ABC may have failed to include the lesion in the temporal lobe as part of the WM volume. This did not occur during the segmentation of the volume acquired during the follow-up scan, where this region seems to have been more appropriately segmented (see arrows).
Longitudinal comparison of TBI using Slicer 3.6
Few non-commercial software tools are available to help clinicians analyze and solve problems of quantitative analysis and visualization. Problems on which there has been significant progress up to this point include data processing challenges, problems recognizing acute versus chronic phases of traumatic brain injury, establishing the means of performing more sensitive quantification of change, and determining extent of cortical and ventricular injury, amount of white matter injury and axonal damage and the means of associating change TBI morphometry over time with clinical outcome.
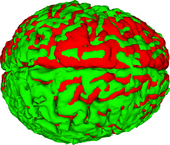
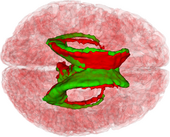
To date, the UCLA team has successfully performed co-registration of several baseline and follow-up TBI volumes, classification of healthy and injured tissues, as well as longitudinal analysis of TBI cases. Specifically, we have introduced the combined the use of multimodal TBI segmentation and longitudinal analysis using 3D Slicer. For three representative TBI cases, semi-automatic tissue classification and 3D model generation have been performed to assess longitudinal TBI evolution using multimodal volumetrics and clinical atrophy measures. Identification and quantitative assessment of extra- and intra-cortical bleeding, lesions, edema and diffuse axonal injury was also performed. 3D Slicer tools have been used to perform cross-correlation of multimodal metrics from structural imaging (structural volume, atrophy measurements, etc.) and with clinical outcome variables (time since injury, age, gender, etc.) and other potential factors predictive of recovery.
3D Slicer workflows have been found to be suitable for TBI clinical practice and patient monitoring, particularly for assessing damage extent as well as for the measurement of neuroanatomical change over time. With knowledge of general location, extent, and degree of change, such metrics computed in 3D Slicer can be associated with clinical measures and subsequently used to suggest viable treatment options for individual subjects against patterns that are typical TBI populations. Thus, the methodology that has been demonstrated up to this point using the 3D Slicer platform has the potential for significant impact upon the state of the art in TBI neuroimaging as well as upon the added benefit of TBI neuroimaging techniques from the standpoint of clinical monitoring, diagnosis and treatment.
Shown below are four images that are illustrative of this procedure for Patient 3 (MR and CT data available for download from above). A more comprehensive description of this analysis will very soon be made available in a manuscript to be submitted for peer review.
In conclusion, although the UCLA team is only 4 months into the first year of participating in the NA-MIC project, we have not only already fulfilled all specific aims for Year 1, but also made a significant amount of progress beyond these aims.
3D Slicer as a software platform for TBI
To address the urgent need for clinician-friendly TBI analysis tools, we have combined the use of multimodal, semi-automatic TBI analysis methods within 3D Slicer. To showcase the ability of the UCLA team to perform quantitative longitudinal analysis of TBI in 3D Slicer, we have analyzed three cases of semi-automatic TBI volume segmentation and 3D brain model generation while also highlighting the added clinical insight which 3D Slicer can offer.
Slicer 3 has the capability of providing visual assessment of multimodality imaging of 3D fiber tracts and morphometry in TBI. It provides the possibility for potential identification of specific targets for neurological testing enabling the clinician or researcher to deploy tests based on hypotheses derived from image analysis. Ultimately, through a more principled approach, quantitative assessments can be made.
Over the past 4 months, the UCLA team has developed a sophisticated protocol for image segmentation and model generation, which has been applied to three representative TBI patients with spectacular results. This standard protocol has been confirmed to be optimal for TBI case analysis in 3D Slicer. Specifically, brain lesions adjacent to CSF were segmented from volumes acquired using FLAIR, GRE imaging, TSE T2-weighted volumes as well as DWI. Because SWI is generally superior to GRE and T2-weighted imaging to detect hemorrhagic lesions, volumes acquired using the former modality were used to identify micro-hemorrhages. Images that were additionally available in the context of our protocol were used to confirm segmentation accuracy as well as to illustrate the additional capabilities of 3D Slicer to segment images from a variety of MR data sets and combination of sequences. Throughout the past several months, the UCLA team has demonstrated the usefulness of semi-automatic segmentation tools available in 3D Slicer software, including the Atlas Based Classification (ABC) segmenter. As opposed to other specialized segmenters where access is often restricted from outside users, the ABC segmenter is freely available as a segmentation module in 3D Slicer. The method is automatic, its execution requires minimal user supervision, and its appropriateness for TBI case analysis is excellent. In addition, the ABC segmenter possesses the ability to perform co-registration of an arbitrary number of MR volumes acquired using various sequences. This makes ABC highly suitable to the UCLA multimodal TBI imaging paradigm, where as many as 12 distinct sequence types are employed in the context of a sophisticated TBI analysis protocol. At UCLA, tissue-type segmentation has already been used to calculate the total volumes of selected structure types (ventricular system, non-hemorrhagic lesions, and hemorrhagic lesions, white matter and gray matter). Volume changes have been computed as the ratio of the difference in volume between the follow-up and acute baseline time points, to the volume at the latter time point. In addition to these measures, the UCLA team has also computed five measures of atrophy, namely the bifrontal index, the bicaudate index, Evan’s index, the ventricular index and Huckman’s index. These measures as computed in Slicer have been found to be in excellent agreement with previous results available in the TBI literature.
In conclusion, over the past 4 months, we have used Slicer 3 to perform multimodal data fusion (linear co-registration, segmentation using ABC, etc.). Tissue classification with normal atlas prior, deformable (fluid) atlas to subject registration, as well as segmentation of lesions, bleedings, shunts has also been performed.
Despite appreciable recent efforts to integrate advanced neuroimaging analysis with existing methodologies for TBI treatment, there has been insufficient progress in combining personalized case description and characterization with surgical and neuro-intensive care methods. Specifically, an important challenge encountered in the attempt of performing such integration is the difficulty of determining how each subject’s lesion profile modulates brain atrophy, and how these changes lead to behavioral, cognitive and neural dysfunction. In TBI, significant additional difficulties exist because (1) damage is often inflicted upon more than a single functional area, and additionally because (2) injuries can affect brain regions and structures whose detailed functions have not been studied and quantified as rigorously as those mentioned above. The pervasive presence of diffuse axonal injury (DAI) in TBI can lead to additional functional changes which are strongly modulated by white matter (WM) connectivity and which can be very difficult to quantify. For these reasons, TBI is considerably more challenging to study than many other conditions of the diseased brain, both methodologically and conceptually. One area of progress for the UCLA DBP group involves a methodological framework for patient-tailored structural characterization of TBI-related brain atrophy which combines magnetic resonance imaging (MRI) with image processing methods to perform patient-specific longitudinal analysis of TBI brain morphometry. These methods can be used to determine how atrophy differentially affects the TBI brain depending on injury location, and how such atrophy evolves longitudinally compared to normative samples of healthy adults. This contribution provides proof of concept in favor of the fact that our methods implemented via 3D Slicer can substantially aid in the process of pursuing such hypothesis-driven research.
EEG/MRI source localization in TBI patients
Though an appreciable number of traumatic brain injury (TBI) patients with post-traumatic epilepsy (PTE) may benefit from epileptogenic focus removal, the localization of epileptic foci remains difficult in PTE. This difficulty is partly due to the complexity of TBI-related structural brain changes, and is currently seen as deterrent to surgery. One area of progress by the UCLA DBP group involves determining the effects of TBI-related pathology upon EEG source localization accuracy in acute TBI. Realistic models of the head with 25 tissue types (including 6 types accounting for TBI pathology) are generated using 3D Slicer based on multimodal MRI via the finite element method (FEM). This research involving 3D Slicer has helped us to determine that TBI-related changes in the conductivity profile of the head can have appreciable effects upon EEG source localization, and that such changes should therefore be accounted for when performing forward/inverse modeling.
Outreach
Our outreach goals include:
- TBI Cases TBI Registration Case Library
- Develop comprehensive tutorial/how-to guide
- Design user friendly TBI workflow interface for Slicer
- Presentations/posters at OHBM, SFN, and other (inter)national meetings in year 2
- Hands-on teaching event for the DBP scientific community for year 3
- Peer reviewed publications
Outreach Events
UCLA Neurology Science Day (January 2011)
The UCLA Department of Neurology held its Third Annual Neurology Science Day on Wednesday, January 26, 2011. During the Poster Session, Andrei Irimia presented a poster to the Neurology Faculty at UCLA.
File:Irimia-UCLA-Neurology-Day-poster.pdf
TBI DBP Meeting at NA-MIC AHM (January 2011)
The UCLA and SCI teams had several fruitful and friendly meetings during the All Hands Meeting in Salt Lake City. The first of these meetings was attended by about 30 researchers, including Guido Gerig, Marcel Prastawa, Bo Wang, Sylvain Gouttard, Andrei Irimia, Micah Chambers, Stephen Aylward, Hans Johnson, and their teams. This part of the meeting focused on how Slicer tools can be used to study pathology, with a focus on Huntington Disease and TBI. In the opening of the meeting, Guido raised the question of what Slicer tools are already available to assess longitudinal changes. Hans Johnson expressed his interest in Slicer and commented on the possible activity of using the platform for the development of clinical trials.
For the TBI project, the Utah team is interested in obtaining radiological TBI case descriptions from UCLA radiologists and in having more input from UCLA as to how various types of TBI images (e.g. Flair, GRE bleed, etc.) should be interpreted. Such radiological case descriptions would allow one to better interpret TBI data and to determine the class of pathology to which various features belong, based on a comparative examination of different scans. Another request from the Utah team is to have patient histories for the subjects that we provide for them. They would like to use this information in conjunction with the case descriptions to learn more about the type of lesions that they are studying, and to obtain a sense of how the patient history and case evolution is reflected in the anatomical changes that are apparent from the scans.
One concern that was expressed regards the ability of this project's time frame to accommodate both algorithm development as well as the development of clinically oriented tools and measures which require the output of the former from the very beginning. For example, we need to develop longitudinal analysis tools but the algorithms to do TBI segmentation are a prerequisite to this, although it may take years to develop the latter. Andrei pointed out to the possibility of using mild TBI cases in the beginning in order to develop longitudinal analysis tools, while the Utah team is developing more complex and robust methods that can handle difficult cases.
Five goals of clinical interest were discussed during the meetings, namely (1) the ability to do TBI tissue classification, (2) the ability to perform volumetric analysis to allow for neuroanatomic assessment, (3) the ability to track the fate of lesions and pathology using automatic segmentation, (4) the ability to generate quantitative output in the form of a report to demonstrate that the use of imaging correlates with improvement in outcome scores, and (5) the ability to easily quantify WM tract distortion and change, as well as how this distortion evolves over time.
One item that was pointed out to the entire audience is that the focus of Slicer is on subject-level rather than population-level analysis, in spite of existing clinical interest in performing statistical studies of population groups. However, one item which clinicians would find appealing is precisely the ability to compute anatomical measures at the subject level, particularly because these subject-level measures can then be used for population-level statistical analysis outside Slicer. Although such population-level analyses may not be within the scope of Slicer, it may be useful to take their specifications into account in the context of formulating goals and strategies for the collaboration.
ABC segmentations of TBI volumes were reviewed in a separate session at the meeting, and a number of plans for the future were formulated. One item that was discussed was the selective use of image channels to perform TBI segmentation. Depending on the type of pathology that is the subject of focus, it may be of interest to include in the segmentation process only those scans in which the pathology is most obvious. The two teams decided to collaborate on how best to accomplish this.
A number of technicalities related to ABC and to segmentation in general were discussed, with the end conclusion being that the results thus far generated with ABC can probably be much improved upon after some exploratory analysis. Team members agreed to keep in touch by email, phone, teleconference, etc. It was agreed upon that there should be some type of periodical face-to-face interaction between the teams at UCLA and SLC, possibly every several months.
TBI DBP Conference Call with Utah Team (September 9, 2011)
The UCLA and Utah teams had a productive conference call on September 9, 2011. All progress up to this date was reviewed, including (1) integration of MRI Watcher into Slicer, (2) the upcoming version of Slicer in QT, (3) the conference paper that was submitted to SPIE, and (4) the availability of CT data for TBI patients. The two teams also reviewed various technical items, including (5) the calculation and display of Jacobian deformation maps for TBI between acute and chronic time points for use by clinicians, (6) the issue of how to address changes in topology between time points, (7), possible relaxation of diffeomorphic constraints for the purpose of quantifying the deformation field, (8), the step-by-step TBI tutorial that was presented by Andrei Irimia at the Boston June Meeting, (9) possible future coordination between the Utah and UNC/Kitware/GA Tech teams. The overall conclusion from the meeting was that much progress has been achieved this year and that we are looking forward to presenting our accomplishments in Salt Lake City at the Annual All-Hands Meeting.
NA-MIC Conference Call (October 27, 2011)
During the NA-MIC conference call with Dr. Kikinis and his team at BWH, Dr. Van Horn highlighted our excellent research progress throughout the past year, including publication of a paper in the Journal of Neurotrauma that uses Slicer, one publication accepted for MICCAI 2012 based on a study directed by Guido Gerig at the University of Utah, two manuscripts on TBI geometric metamorphosis based on research directed by Stephen Aylward from Kitware, one paper based on research directed by Yifei Lou and Allen Tannenbaum on deformable registration, and other conference abstracts and posters.
TBI DBP Conference Call (November 10, 2011)
A conference call was held with the Kitware, GA Tech and Utah teams regarding activities planned for the NA-MIC All Hands Meeting in Salt Lake City. While there, the three teams will collaborate on atlas based classification, nonrigid registration algorithms, and on several manuscripts in progress.
NA-MIC Conference Call (November 16, 2011)
Dr. Van Horn had a conference call with Tina Kapur regarding the upcoming meeting in January. Our recent progress was highlighted, including the publication of a paper in the Journal of Neurotrauma, conference abstracts and proceedings, posters and other activities.
UCLA visit by Dr. Guido Gerig from Univ. of Utah (May 22, 2012)
Dr. Guido Gerig visited UCLA and presented his group's research to members of LONI as well as to Dr. Paul Vespa and to his colleagues at the Neurointensive Care Unit (NICU) of the UCLA Ronald Reagan Medical Center. The two groups discussed the application of Dr. Gerig's TBI registration algorithms to the UCLA data, and brainstormed with regard to possible avenues for future collaboration. It was decided to share additional data between the two groups as they become available. Dr. Gerig also met with Dr. Arthur Toga at the LONI and with Dr. Jeff Alger at the Brain Mapping Center. This was a very welcome and excellent visit that resulted in much progress with regard to future work by the two groups.
NA-MIC All Hands Meeting (January 2013)
Dr. John D. Van Horn presented our latest research at the 2013 All Hands Meeting in Salt Lake City. The slides of his talk are available below.
UCLA-HMS-Utah Collaborative Meeting (April 2013)
Andrei Irimia and Micah Chambers (UCLA) and Dr. Ron Kikinis (HMS) travelled to Salt Lake City in order to set goals for the following few months before the Summer Project Week to take place in Boston in June 2013. Ron emphasized the need for a custom module in Slicer which can do TBI segmentation, and the question was raised by the Utah team regarding how many time points and modalities the module should be able to accommodate. It was also pointed out that the registration part of the module is already available in ABC, and Ron suggested that the module should be made as simple as possible so that it can be delivered to UCLA in a timely fashion. He also suggested that the number of user interactions should be minimized and that most decisions should be made by the developers (the Utah Team). An overview of ongoing work was also made, including the MICCAI submission this year as well as the implementation of a parcellation map for each longitudinal time point. The Utah team outlined the need to convert the core algorithm to ITK, and then from ITK to Slicer. Guido Gerig pointed out that the greatest challenge is the interaction, and Ron demonstrated the cube functionality in Slicer, which will allow the Utah team to circumvent this challenge. Another idea that was passed around was regarding the calculation of cortical thickness to produce a visualization of it and have that in Slicer as well. The developed module should obey Ron's rules for tools.
At the end of the meeting, it was decided that the Utah team would convert the algorithm from Matlab to C++, and integrate it with Slicer during project week with Steve Pieper's help. Then the module will be made available to the UCLA team, and a demonstration of its functionality should be made during the Slicer event at UCLA in July. Ron added that there should be papers by the Utah team on the algorithm itself and by the UCLA team on its application (but only once it's available to UCLA). The UCLA team will test the module and will suggest areas in need for improvement.
USC Workshop on 3D Slicer for Brain research (February 2013)
File:INI-neuroimaging-workshop-flyer.pdf
The objective of the workshop is to introduce the capabilities of the 3D Slicer open-source software for medical image analysis and 3D visualization. The workshop is divided into two parts: the first part introduces the basics of 3D visualization of DICOM images and Diffusion Tensor Image Analysis within the platform, and the second part introduces the 3D Slicer capabilities for Traumatic Brain Injury research. Intended audience: neuroscience and biomedical engineering graduate students, postdoctoral scholars, clinicians and faculty. For more information:
Investigators
USC
* John Darrell Van Horn, M.Eng., Ph.D. - Principal Investigator of the DBP * Andrei Irimia, Ph.D. - assistant professor, USC [2] * Arthur W. Toga, Ph.D. (investigator)
UCLA
* Paul Vespa, M.D., F.C.C.M., F.A.A.N. (investigator) * Jeffry Alger, Ph.D. (investigator)
University of Utah
* Guido Gerig, Ph.D. (lead technical contact) * Bo Wang, B.S. (graduate student)
Kitware/UNC Chapel Hill
* Stephen Aylward, Ph.D. (director of medical imaging) * Martin Styner, Ph.D. (lead algorithm and engineering contact)
Stony Brook University
* Allen Tannebaum, Ph.D. (Principal Investigator of the Algorithm Core)
Harvard Medical School
* Ron Kikinis, M.D. (Principal Investigator) * Sonja Pujol, Ph.D.
Awards, Honors and Accomplishments
- Research using 3D Slicer was honored with the Mazziotta Prize awarded to Andrei Irimia for excellence in postdoctoral research in the field of neurology
- Review on the use of 3D Slicer for TBI outcome prediction was selected as the inaugural article published by NeuroImage: Clinical
- Over 10,000 downloads of the PLoS ONE research article co-authored on Phineas Gage by the UCLA group and featuring 3D Slicer
- Research involving 3D Slicer performed by the UCLA group on Phineas Gage was featured extensively as main article by Discover Magazine
- Andrei Irimia received the Young Investigator Award from the American College of Neuropsychopharmacology (ACNP) for work in 3D Slicer (given to only 10 out of 200 applicants in 2012)
- Connectomics visualization and work in 3D Slicer by the UCLA group was featured at the Ars Electronica 2012 Conference in Linz, Austria
- Andrei Irimia was awarded a research travel fellowship by the Brain Injury Research Center at UCLA for his TBI research in Slicer
- Travel scholarship was awarded to Andrei Irimia for presenting 3D Slicer research at the Dynamics Days 2012 conference in Baltimore, MD
- Scientific visualizations based on 3D Slicer featured in the 2012 and 2013 calendars of the UCLA Brain Research Institute
- TBI work in 3D Slicer is recognized at the research competition finalist stage (top 15 of 400 participants) at the Neurotrauma Symposium, Phoenix, AZ
- Andrei Irimia was awarded a scholarship to attend the Neurotrauma Symposium in Phoenix, AZ to present his Slicer research (top 10 of 390 applicants)
- Article by UCLA group on 3D Slicer was featured in the top 12 most downloaded articles published by the journal NeuroImage
- Andrei Irimia was selected as research competition finalist for his TBI research in Slicer from among 390 participants at the Neurotrauma Symposium
- Andrei Irimia obtained the First Prize in the Summer Tutorial Contest of the National Alliance for Medical Image Computing [3]
- Andrei Irimia's visualization of TBI using Slicer has been selected to be featured on the cover of the Journal of Neurotrauma for a special issue on bioengineering for TBI
- Andrei Irimia was awarded the first prize in the Fine Science Award Competition by the Brain Research Institute at UCLA for excellence in postdoctoral neuroscience research
- Andrei Irimia obtained a competitive travel award to present TBI research at a Keystone Symposium on the Molecular and Clinical Biology of TBI to be held in Keystone, Colorado in February 2012
- Andrei Irimia obtained a travel scholarship to present a TBI-related poster at the Dynamic Days 2012 conference to be held in Baltimore, MD in January 2012
Publications
Journal Articles
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson, Paul M. Vespa and John D. van Horn (2014) Structural and connectomic neuroimaging for the personalized study of longitudinal alterations in cortical shape, thickness and connectivity after traumatic brain injury Journal of Neurosurgical Sciences (accepted)
- Sheng-Yang M. Goh, Andrei Irimia, Carinna M. Torgerson and John D. van Horn (2014) Neuroinformatics challenges to the structural, connectomic, functional and electrophysiological multimodal imaging of traumatic brain injury Frontiers in Neuroinformatics volume 8, article 19, 12 pages [4]
- Andrei Irimia and John D. van Horn (2014) Systematic network lesioning reveals the core white matter scaffold of the human brain Frontiers in Human Neuroscience volume 8, article 51, 14 pages [5]
- Matthew J. Wright, David L. McArthur, Jeffry R. Alger, John D. van Horn, Andrei Irimia, Maria Filippou, Thomas C. Glenn, David A. Hovda and Paul M. Vespa (2013) Early metabolic crisis-related brain atrophy and cognition in traumatic brain injury Brain Imaging and Behavior volume 7, pages 307-315 [6]
- Andrei Irimia, Sheng-Yang M. Goh, Micah C. Chambers, Carinna M. Torgerson, Nathan R. Stein, Paul M. Vespa and John D. van Horn (2013) Electroencephalographic brain activity localization in acute traumatic brain injury as a guide to surgery, monitoring and treatment Clinical Neurology and Neurosurgery volume 115, pages 2159-2165 [7]
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson, Micah C. Chambers, Ron Kikinis and John D. van Horn (2013) Forward and inverse electroencephalographic modeling in acute traumatic brain injury Clinical Neurophysiology volume 124, pages 2129-2145 [8]
- Yifei Lou, Andrei Irimia, Patricio A. Vela, Micah C. Chambers, John D. van Horn, Paul M. Vespa and Allen R. Tannenbaum (2013) Multimodal deformable registration of traumatic brain injury MR volumes via the Bhattacharyya distance IEEE Transactions on Biomedical Engineering volume 60, pages 2511-2520 [9]
- Andrei Irimia and John D. van Horn (2012) The structural, connectomic and network covariance of the human brain NeuroImage, volume 66, pages 489-499 [10]
- Andrei Irimia, Bo Wang, Stephen R. Aylward, Marcel W. Prastawa, Danielle F. Pace, Marc Niethammer, Guido Gerig, David A. Hovda, Ron Kikinis, Paul M. Vespa and John D. van Horn (2012) Multimodal neuroimaging of structural pathology and connectomics in traumatic brain injury: toward personalized outcome prediction Neuroimage: Clinical volume 1, pages 1-17 [11]
- John D. van Horn, Andrei Irimia, Carinna M. Torgerson, Micah C. Chambers, Arthur W. Toga (2012) Mapping connectivity damage in the case of Phineas Gage. Plos ONE volume 7, article e37454 [12]
- Andrei Irimia, Micah C. Chambers, Carinna M. Torgerson and John D. van Horn (2012) Circular representation of human cortical networks for subject and population-level connectomic visualization NeuroImage volume 60, pages 1340-1351
- Andrei Irimia, Micah C Chambers, Carinna M Torgerson, Maria Filippou, David A Hovda, Jeffry R Alger, Guido Gerig, Arthur W Toga, Paul M Vespa, Ron Kikinis, John D Van Horn (2012) Patient-tailored connectomics visualization for the assessment of white matter atrophy in traumatic brain injury. Frontiers in Neurology volume 3, article 1, 21 pages [13]
- Andrei Irimia, Micah C. Chambers, Jeffry R. Alger, Maria Filippou, Marcel W. Prastawa, Bo Wang, David A. Hovda, Guido Gerig, Arthur W. Toga, Ron Kikinis, Paul M. Vespa, John D. van Horn (2011) Comparison of acute and chronic traumatic brain injury using semi-automatic multimodal segmentation of MR volumes. Journal of Neurotrauma volume 28, pages 2287-2306 [14]
Proceedings
- Bo Wang, Wei Liu, Marcel W. Prastawa, Andrei Irimia, Paul M. Vespa, John D. Van Horn, P. Thomas Fletcher and Guido Gerig (2014) Four dimensional active cut: an interactive tool for pathological anatomy modeling Proceedings of the Twelfth International Symposium on Biomedical Imaging (ISBI 2013), April 29-May 2, 2014, Beijing, China
- Bo Wang, Marcel W. Prastawa, Andrei Irimia, Micah C. Chambers, Paul M. Vespa, John D. van Horn and Guido Gerig (2012) Segmentation of MRI presenting pathology and inconsistent multimodal information. Proceedings of the Fifteenth International Conference on Medical Image Computing and Computer-Assisted Intervention (MICCAI 2012), October 1-5, 2012, Nice, France.
- Bo Wang, Marcel W. Prastawa, Avishek Saha, Suyash P. Awate, Andrei Irimia, Micah C. Chambers, Paul M. Vespa, John D. van Horn, Valerio Pascucci and Guido Gerig (2013) Modeling four-dimensional changes in pathological anatomy using domain adaptation: analysis of traumatic brain injury imaging using a tumor database Proceedings of the Third International Workshop on Multimodal Brain Image Analysis (MBIA 2013), September 22-26, 2013, Nagoya, Japan Also published in Lecture Notes in Computer Science, volume 8159, pages 31-39
- Sheng-Yang M. Goh, Andrei Irimia, Carinna M. Torgerson, Ron Kikinis, Paul M. Vespa and John D. van Horn (2013) High-resolution electroencephalographic forward modeling in traumatic brain injury using the finite element method Proceedings of the Eleventh International Symposium on Biomedical Imaging (ISBI 2013), April 7-11, 2013, San Francisco, California, USA
- Bo Wang, Marcel W. Prastawa, Andrei Irimia, Micah C. Chambers, Paul M. Vespa, John D. van Horn and Guido Gerig (2013) Analyzing imaging biomarkers for traumatic brain injury using four-dimensional modeling of longitudinal magnetic resonance imaging Proceedings of the Eleventh International Symposium on Biomedical Imaging (ISBI 2013), April 7-11, 2013, San Francisco, California, USA
- Bo Wang, Marcel W. Prastawa, Suyash P. Awate, Andrei Irimia, Micah C. Chambers, Paul M. Vespa, John D. Van Horn and Guido Gerig (2012) Segmentation of serial MRI of TBI patients using personalized atlas construction and topological change estimation Proceedings of the Tenth International Symposium on Biomedical Imaging (ISBI 2012), May 2-5, 2012, Barcelona, Catalonia, Spain
- Bo Wang, Marcel W. Prastawa, Andrei Irimia, Micah C. Chambers, Paul M. Vespa, John D. van Horn, Guido Gerig (2012) A patient-specific segmentation framework for longitudinal MR images of traumatic brain injury Proceedings of the Twenty-Fifth International Conference of SPIE—The International Society for Optical Engineering, February 4-9, 2012, San Diego, California, USA
- Marc Niethammer, Gabriel L. Hart, Danielle F. Pace, Micah C. Chambers, Andrei Irimia, John D. van Horn, Stephen R. Aylward (2011) Geometric metamorphosis. Proceedings of the Fourteenth International Conference on Medical Image Computing and Computer-Assisted Intervention (MICCAI 2011), September 18-22, 2011, Toronto, Ontario, Canada
Abstracts
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson and John D. van Horn (2014) Cortical atrophy and demyelination in Alzheimer’s disease and in traumatic brain injury: a comparative study of structural brain changes using multimodal neuroimaging Proceedings of the Alzheimer’s Association International Conference, July 12-17, 2014, Copenhagen, Denmark.
- Matthew J. Wright, Thomas C. Glenn, David L. McArthur, Jeffry R. Alger, John D. van Horn, Andrei Irimia, Maria Filippou, David A. Hovda and Paul M. Vespa (2014) Multimodal imaging reveals the link between early metabolic crisis and cognitive outcomes following traumatic brain injury Proceedings of the Thirty-Second Annual Symposium of the National Neurotrauma Society, Including the AANS/CNS Joint Section on Neurotrauma and Critical Care, July 1, 2014, Marriott Marquis Hotel, San Francisco, California, USA. Also published in Journal of Neurotrauma.
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson, Bo Wang, Marcel W. Prastawa, Guido Gerig, Paul M. Vespa and John D. van Horn (2014) Brain atrophy mapping in traumatic brain injury using multimodal neuroimaging Proceedings of the Thirty-Second Annual Symposium of the National Neurotrauma Society, Including the AANS/CNS Joint Section on Neurotrauma and Critical Care, June 29-July 2, 2014, Marriott Marquis Hotel, San Francisco, California, USA. Also published in Journal of Neurotrauma.
- Guido Gerig, Bo Wang, Andrei Irimia, Paul M. Vespa, John D. van Horn and Marcel W. Prastawa (2014) Computational considerations in traumatic brain injury neuroimaging data analysis Proceedings of the Thirty-Second Annual Symposium of the National Neurotrauma Society, Including the AANS/CNS Joint Section on Neurotrauma and Critical Care, June 29-July 2, 2014, Marriott Marquis Hotel, San Francisco, California, USA. Also published in Journal of Neurotrauma.
- Sheng-Yang M. Goh, Andrei Irimia, Carinna M. Torgerson, Ron Kikinis, Paul M. Vespa and John D. van Horn (2014) Localization of epileptiform electrical activity recorded from severe traumatic brain injury patients using scalp electroencephalography Proceedings of the Twentieth Annual Meeting of the Organization on Human Brain Mapping (OHBM 2014), June 8-12, 2014, Hamburg, Germany
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson, Paul M. Vespa and John D. van Horn (2014) Multimodal neuroimaging for mapping brain atrophy and axonal demyelination in traumatic brain injury Proceedings of the Twentieth Annual Meeting of the Organization on Human Brain Mapping (OHBM 2014), June 8-12, 2014, Hamburg, Germany
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson and John D. van Horn (2014) Connectomic neuroimaging for estimating effective brain age as a biomarker of neurodegeneration Proceedings of the Twentieth Annual Meeting of the Organization on Human Brain Mapping (OHBM 2014), June 8-12, 2014, Hamburg, Germany
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson, Paul M. Vespa and John D. van Horn (2014) Quantitative assessment of cortical atrophy and axonal demyelination in severe traumatic brain injury using multimodal neuroimaging Proceedings of the Annual Meeting of the International Neurotrauma Society (INTS 2014), March 19-23, 2014, Budapest, Hungary. Also published in Journal of Neurotrauma, vol. 31, abstract no. 172
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson, Micah C. Chambers, Paul M. Vespa, Ron Kikinis and John D. van Horn (2013) Electroencephalographic inverse localization of cortical loci generating epileptiform activity in comatose acute traumatic brain injury patients Proceedings of the Forty‐Third Annual Meeting of the Society for Neuroscience (SfN 2013), November 9-13, 2013, San Diego, California, USA
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson, Micah C. Chambers, Paul M. Vespa, Arthur W. Toga, Ron Kikinis and John D. van Horn (2013) Application of electroencephalographic inverse localization methods to study the neural dynamics and information processing capabilities of injured cortical networks Proceedings of the Twentieth Joint Symposium on Neural Computation, June 1, 2013, California Institute of Technology, Pasadena, California, USA
- Sheng-Yang M. Goh, Andrei Irimia, Carinna M. Torgerson, Ron Kikinis, Paul M. Vespa and John D. van Horn (2013) Electroencephalographic forward modeling for the network-theoretic analysis of injury-affected brains using quantitative measures of information processing and macro-scale neural computation Proceedings of the Twentieth Joint Symposium on Neural Computation, June 1, 2013, California Institute of Technology, Pasadena, California, USA
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson, Micah C. Chambers, Nathan R. Stein, Jeffry R. Alger, Paul M. Vespa and John D. van Horn (2013) Inverse localization and monitoring of epileptiform cortical activity in acute traumatic brain injury via electroencephalography Proceedings of the Thirty-First Neurotrauma Symposium, August 4-7, 2013, Gaylord Opryland Resort, Nashville, Tennessee, USA. Also published in Journal of Neurotrauma, volume 39, page A144.
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson, Micah C. Chambers, Bo Wang, Marcel W. Prastawa, Paul M. Vespa, Jeffry R. Alger, Guido Gerig, Stephen R. Aylward, Arthur W. Toga, Ron Kikinis and John D. van Horn (2013) Quantification of longitudinal changes in cortical network circuitry prompted by traumatic brain injury Accepted for publication in the Proceedings of the Workshop on Network Science of the Society for Industrial and Applied Mathematics, July 7-8, 2013, San Diego, California, USA
- Sheng-Yang M. Goh, Andrei Irimia, Carinna M. Torgerson, Ron Kikinis, Paul M. Vespa and John D. van Horn (2013) Impact of brain injury upon the EEG forward solution as computed using the finite element method Proceedings of the Nineteenth Annual Meeting of the Organization on Human Brain Mapping (OHBM 2013), June 16-20, 2013, Seattle, Washington, USA
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson, Ron Kikinis, Paul M. Vespa and John D. van Horn (2013) Effects of traumatic brain injury upon the inverse localization accuracy of electroencephalography Proceedings of the Nineteenth Annual Meeting of the Organization on Human Brain Mapping (OHBM 2013), June 16-20, 2013, Seattle, Washington, USA
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson, Micah C. Chambers, Ron Kikinis, Arthur W. Toga and John D. van Horn (2013) Inverse localization and quantification of epileptiform electrical activity recorded from acute traumatic brain injury patients via electroencephalography Proceedings of the Fifty-Third Annual Meeting of the American Society of Psychopharmacology, May 28-31, 2013, Hollywood, Florida, USA
- Andrei Irimia, Micah C. Chambers, Maria Filippou, Paul M. Vespa, Jeffry R. Alger, David A. Hovda, Arthur W. Toga, Ron Kikinis and John D. van Horn (2013) Effects of traumatic brain injury upon the architecture and nonlinear dynamics of cortical networks Proceedings of the Thirty-First Annual International Conference on Chaos and Nonlinear Dynamics (Dynamics Days 2013), January 3-6, 2013, Denver, Colorado, USA
- Andrei Irimia, Micah C. Chambers, Marcel W. Prastawa, Paul M. Vespa, David A. Hovda, Jeffry R. Alger, Guido Gerig, Stephen R. Aylward, Arthur W. Toga, Ron Kikinis and John D. van Horn (2012) Connectomic analysis of white matter atrophy after severe traumatic brain injury Proceedings of the Fifty-First Annual Meeting of the American College of Neuropsychopharmacology, December 2-6, 2012, Hollywood, Florida, USA
- Andrei Irimia, Micah C. Chambers, Marcel W. Prastawa, Paul M. Vespa, David A. Hovda, Jeffry R. Alger, Guido Gerig, Stephen R. Aylward, Arthur W. Toga, Ron Kikinis and John D. van Horn (2012) Systematic connectomic analysis of white matter atrophy associated with severe traumatic brain injury Proceedings of the Thirtieth Neurotrauma Symposium, July 22-25, 2012, Arizona Biltmore Resort and Spa, Phoenix, Arizona, USA. Also published in Journal of Neurotrauma, volume 29, pages A8-A9.
- Andrei Irimia, John D. van Horn, Micah C. Chambers, Marcel W. Prastawa, Silvain Gouttard, Paul M. Vespa, David A. Hovda, Jeffry R. Algers, Sonia M. A. Pujol, Guido Gerig, Stephen R. Aylward, Arthur W. Toga and Ron Kikinis (2011) Connectome-level evaluation of neurodegeneration caused by traumatic brain injury Proceedings of the Eighteenth Annual Meeting of the Organization on Human Brain Mapping (OHBM 2012), June 10-14, 2012, Beijing, China
- Micah C. Chambers, Andrei Irimia and John D. van Horn (2012) Combined functional and structural connectivity for an improved look at the brain Proceedings of the Nineteenth Joint Symposium on Neural Computation, June 2, 2012, University of California, Riverside, California, USA
- Andrei Irimia, S. Y. Matthew Goh, Carinna M. Torgerson, Micah C. Chambers, David A. Hovda, Jeffry R. Alger, Paul M. Vespa, Guido Gerig, Arthur W. Toga, Ron Kikinis and John D. van Horn (2012) Impact of neurotrauma upon the network architecture and information processing capabilities of the human cortex Proceedings of the Nineteenth Joint Symposium on Neural Computation, June 2, 2012, University of California, Riverside, California, USA
- Andrei Irimia, Micah C. Chambers, Marcel W. Prastawa, Paul M. Vespa, David A. Hovda, Jeffry R. Alger, Guido Gerig, Stephen R. Aylward, Arthur W. Toga, Ron Kikinis, John D. van Horn (2012) Systematic connectomic analysis of white matter atrophy associated with severe traumatic brain injury Proceedings of the Thirtieth Neurotrauma Symposium, July 22-25, 2012, Arizona Biltmore Resort and Spa, Phoenix, Arizona, USA
- Andrei Irimia, John D. van Horn, Micah C. Chambers, Marcel W. Prastawa, Silvain Gouttard, Paul M. Vespa, David A. Hovda, Jeffry R. Algers, Sonia M. A. Pujol, Guido Gerig, Stephen R. Aylward, Arthur W. Toga and Ron Kikinis (2011) Connectome-level evaluation of neurodegeneration caused by traumatic brain injury Proceedings of the Eighteenth Annual Meeting of the Organization on Human Brain Mapping (OHBM 2012), June 10-14, 2012, Beijing, China
- Andrei Irimia, SY Matthew Goh, Carinna M. Torgerson, Micah C. Chambers, Jeffry R. Alger, David A. Hovda, Paul M. Vespa, Arthur W. Toga, Ron Kikinis and John D. van Horn (2012) Connectome-level quantification of longitudinal changes in brain circuitry: a study of human neurodegeneration caused by traumatic brain injury Accepted for publication in the Proceedings of the Annual Keystone Conference on Synapses and Circuits: From Formation to Disease, April 1-6, 2012, Steamboat Resort, Steamboat Springs, Colorado, USA
- Andrei Irimia, Micah C. Chambers, Jeffry R. Alger, David A. Hovda, Paul M. Vespa, Arthur W. Toga, Ron Kikinis and John D. van Horn (2012) Patient-tailored longitudinal quantification of brain atrophy in chronic traumatic encephalopathy using multimodal neuroimaging Proceedings of the Annual Keystone Conference on the Clinical and Molecular Biology of Acute and Chronic Traumatic Encephalopathies, February 26-March 2, 2012, Keystone Resort, Keystone, Colorado, USA
- Andrei Irimia, Micah C. Chambers, Maria Filippou, Paul M. Vespa, Jeffry R. Alger, David A. Hovda, Arthur W. Toga, Ron Kikinis, John D. van Horn (2012) Impact of traumatic brain injury upon the architecture and longitudinal dynamics of cortical networks Proceedings of the Thirtieth Annual International Conference on Chaos and Nonlinear Dynamics (Dynamics Days 2012), January 4-7, 2012, Baltimore, Maryland, USA
- Andrei Irimia, Micah C. Chambers, Maria Filippou, Jeffry R. Alger, Marcel W. Prastawa, Bo Wang, Silvain Gouttard, Sonia M. A. Pujol, Stephen R. Aylward, David A. Hovda, Guido Gerig, Arthur W. Toga, Ron Kikinis, Paul M. Vespa and John D. van Horn (2011) Quantification of morphometric and volumetric changes associated with recovery from traumatic brain injury using clinical atrophy measures Neuroscience Poster Session, Brain Research Institute, Ackerman Student Union Grand Ballroom, University of California, Los Angeles, November 29, 2011, Los Angeles, California, USA
- Andrei Irimia, Micah C. Chambers, Paul M. Vespa, Arthur W. Toga, John D. van Horn (2011) Cortical network visualization and analysis in traumatic brain injury using multimodal neuroimaging Proceedings of the Eighteenth Joint Symposium on Neural Computation, June 4, 2011, Institute of Neural Computation, University of California, San Diego, La Jolla, California, USA
- Andrei Irimia, Micah C. Chambers, Maria Filippou, Jeffry R. Alger, Marcel W. Prastawa, Bo Wang, Silvain Gouttard, Sonia M. A. Pujol, Stephen R. Aylward, David A. Hovda, Guido Gerig, Arthur W. Toga, Ron Kikinis, Paul M. Vespa, John D. van Horn (2011) Three‐dimensional calculation and quantification of morphometric and volumetric cortical atrophy indices of widespread clinical use from MRI volumes of traumatic brain injury using 3D Slicer Proceedings of the Forty‐First Annual Meeting of the Society for Neuroscience (SfN 2011), November 12-16, 2011, Washington, District of Columbia, USA
- Andrei Irimia, John D. van Horn, Micah C. Chambers, Marcel W. Prastawa, Silvain Gouttard, Paul M. Vespa, David A. Hovda, Jeffry R. Algers, Sonia M. A. Pujol, Guido Gerig, Stephen R. Aylward, Arthur W. Toga, Ron Kikinis (2011) Automatic multimodal MR image segmentation for the clinical assessment of traumatic brain injury in 3D Slicer Proceedings of the Seventeenth Annual Meeting of the Organization on Human Brain Mapping (OHBM 2011), June 26-30, 2011, Quebec City, Canada
Presentations and Dissemination Events
- Bo Wang, Marcel W. Prastawa, Andrei Irimia, Guido Gerig and John D. van Horn (2014) Interactive segmentation for traumatic brain injury using PARSER: pathological anatomy regression via segmentation and registration Project activity presentation at the Ninth Annual Project Week of the National Alliance for Medical Image Computing (NA-MIC), June 23-27, 2014, Greer Hall, Massachusetts Institute of Technology, Cambridge, Massachusetts, USA
- Matthew J. Wright, Thomas C. Glenn, David L. McArthur, Jeffry R. Alger, John D. van Horn, Andrei Irimia, Maria Filippou, David A. Hovda and Paul M. Vespa (2014) Early metabolic crisis and cognition in traumatic brain injury Session on Advances in Multimodal Imaging of Traumatic Brain Injury, Thirty-Second Annual Symposium of the National Neurotrauma Society, Including the AANS/CNS Joint Section on Neurotrauma and Critical Care, July 1, 2014, Marriott Marquis Hotel, San Francisco, California, USA.
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson, Bo Wang, Marcel W. Prastawa, Guido Gerig, Paul M. Vespa and John D. van Horn (2014) Assessing connectomic alterations in acute and chronic traumatic brain injury and its role in outcome prediction Session on Advances in Multimodal Imaging of Traumatic Brain Injury, Thirty-Second Annual Symposium of the National Neurotrauma Society, Including the AANS/CNS Joint Section on Neurotrauma and Critical Care, July 1, 2014, Marriott Marquis Hotel, San Francisco, California, USA.
- Guido Gerig, Bo Wang, Andrei Irimia, Paul M. Vespa, John D. van Horn and Marcel W. Prastawa (2014) Traumatic brain injury neuroimaging data analysis platform for automatic segmentation of brain lesions Session on Advances in Multimodal Imaging of Traumatic Brain Injury, Thirty-Second Annual Symposium of the National Neurotrauma Society, Including the AANS/CNS Joint Section on Neurotrauma and Critical Care, July 1, 2014, Marriott Marquis Hotel, San Francisco, California, USA.
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson, Paul M. Vespa, Arthur W. Toga and John D. van Horn (2014) Assessing cortical atrophy, axonal demyelination and white matter integrity in traumatic brain injury using magnetic resonance imaging and diffusion tensor imaging Invited presentation at the Annual Meeting of the International Neurotrauma Society (INTS 2014), March 20, 2014, Budapest, Hungary.
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson, Bo Wang, Marcel W. Prastawa, Guido Gerig and John D. Van Horn (2014) Brain imaging, informatics and connectomics in traumatic brain injury: visualization, medical image analysis and translational research using 3D Slicer Workshop and Tutorial on Medical Imaging and Visualization “Structural and diffusion brain imaging for medical image analysis in 3D Slicer” Institute for Neuroimaging and Informatics, February 14, 2014, Soto Building, Keck School of Medicine, University of Southern California, Los Angeles, California, USA
- Bo Wang, Marcel W. Prastawa, Andrei Irimia, John D. van Horn and Guido Gerig (2014) Testing an interactive grab cut segmentation algorithm for traumatic brain injury Project activity presentation at the Tenth All Hands Meeting of the National Alliance for Medical Image Computing (NA-MIC), January 6-11, 2014, Marriott City Center Hotel, Salt Lake City, Utah, USA
- Anuja Sharma, Andrei Irimia, Bo Wang, John D. van Horn, Martin A. Styner and Guido Gerig (2014) Patient-specific longitudinal diffusion tensor imaging analysis in traumatic brain injury Project activity presentation at the Tenth All Hands Meeting of the National Alliance for Medical Image Computing (NA-MIC), January 6-11, 2014, Marriott City Center Hotel, Salt Lake City, Utah, USA
- Andrei Irimia, Sheng Yang Matthew Goh, Carinna M. Torgerson and John D. van Horn (2014) Mapping the effect of traumatic brain injury upon white matter connections in the human brain using 3D Slicer Project activity presentation at the Tenth All Hands Meeting of the National Alliance for Medical Image Computing (NA-MIC), January 6-11, 2014, Marriott City Center Hotel, Salt Lake City, Utah, USA
- Andrei Irimia, Sheng Yang Matthew Goh, Carinna M. Torgerson and John D. van Horn (2014) Systematic evaluation of axonal demyelination subsequent to traumatic brain injury using structural T1- and T2-weighted magnetic resonance imaging Project activity presentation at the Tenth All Hands Meeting of the National Alliance for Medical Image Computing (NA-MIC), January 6-11, 2014, Marriott City Center Hotel, Salt Lake City, Utah, USA
- Andrei Irimia, Sheng Yang Matthew Goh, Carinna M. Torgerson and John D. van Horn (2014) Multimodal neuroimaging for the quantification of brain atrophy at six months following severe traumatic brain injury Project activity presentation at the Tenth All Hands Meeting of the National Alliance for Medical Image Computing (NA-MIC), January 6-11, 2014, Marriott City Center Hotel, Salt Lake City, Utah, USA
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson, Paul M. Vespa and John D. Van Horn (2013) Neuroimaging, geometric modeling and neuroinformatics of traumatic brain injury: developing next-generation visualization and analysis paradigms for clinical use Computer science departmental seminar, State University of New York at Stony Brook, December 4, 2013
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson, Micah C. Chambers, Nathan R. Stein, Jeffry R. Alger, Paul M. Vespa, Ron Kikinis and John D. Van Horn (2013) Finite element geometric modeling of traumatic brain injury for the inverse localization of electrical brain activity recorded using electroencephalography Presentation at the SIAM Conference on Geometric and Physical Modeling (GD/SPM 2013), November 11-14, 2013, Curtis-Double Tree by Hilton Hotel, Denver, Colorado, USA
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson and John D. Van Horn (2013) Biostatistics and neuroinformatics of brain connectivity and structure in traumatic brain injury Presentation at the Institute for Neuroimaging and Informatics, University of Southern California, November 6, 2013, Los Angeles, California, USA
- Sheng-Yang M. Goh, Andrei Irimia and John D. van Horn (2013) Longitudinal quantification and visualization of white matter fiber bundle displacement due to intracranial hemorrhage Presentation at the Brain Injury Research Center, Ronald Reagan Medical Center, University of California, Los Angeles, October 8, 2013, Los Angeles, California, USA
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson, Micah C. Chambers, Nathan R. Stein, Jeffry R. Alger, Paul M. Vespa and John D. van Horn (2013) Forward and inverse electroencephalographic modeling and localization of non-periodic epileptiform cortical spiking in acute traumatic brain injury patients Presentation at the Thirty-First Neurotrauma Symposium, August 4-7, 2013, Gaylord Opryland Resort, Nashville, Tennessee, USA.
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson, Micah C. Chambers, Arthur W. Toga, Paul M. Vespa and John D. van Horn (2013) Neuroimaging of structural pathology and connectomics in traumatic brain injury Invited Presentation at the Twenty-Seventh International Congress and Exhibition on Computer Assisted Radiology and Surgery (CARS 2013), June 26-29 2013, Heidelberg Convention Center, Heidelberg, Germany
- Anuja Sharma, Bo Wang, Andrei Irimia, Micah C. Chambers, Guido Gerig and John D. van Horn (2013) Exploring multimodal registration for improved longitudinal modeling of patient-specific 3D diffusion tensor imaging data Project activity presentation at the Eighth Annual Project Week of the National Alliance for Medical Image Computing (NA-MIC), June 17-21, 2013, Greer Hall, Massachusetts Institute of Technology, Cambridge, Massachusetts, USA
- Bo Wang, Marcel W. Prastawa, Andrei Irimia, Micah C. Chambers, Guido Gerig and John D. van Horn (2013) Validation and testing of 3D Slicer modules implementing the Utah segmentation algorithm for traumatic brain injury Project activity presentation at the Eighth Annual Project Week of the National Alliance for Medical Image Computing (NA-MIC), June 17-21, 2013, Greer Hall, Massachusetts Institute of Technology, Cambridge, Massachusetts, USA
- Andrei Irimia, Micah C. Chambers, Ron Kikinis and John D. van Horn (2013) Clinically oriented assessment of local changes in the properties of white matter affected by intra-cranial hemorrhage Project activity presentation at the Eighth Annual Project Week of the National Alliance for Medical Image Computing (NA-MIC), June 17-21, 2013, Greer Hall, Massachusetts Institute of Technology, Cambridge, Massachusetts, USA
- Andrei Irimia, Micah C. Chambers, Ron Kikinis and John D. van Horn (2013) Visualization and quantification of peri-contusional white matter bundles in traumatic brain injury using diffusion tensor imaging Project activity presentation at the Eighth Annual Project Week of the National Alliance for Medical Image Computing (NA-MIC), June 17-21, 2013, Greer Hall, Massachusetts Institute of Technology, Cambridge, Massachusetts, USA
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson, Micah C. Chambers, Ron Kikinis, Arthur W. Toga and John D. van Horn (2013) Epileptiform electrical activity localization in acute traumatic brain injury using electroencephalographic recordings Presentation at the Fifty-Third Annual Meeting of the American Society of Psychopharmacology: “Recognizing unmet needs in Psychopharmacology: From biomarkers to breakthrough therapies”, May 28-31, 2013, Hollywood, Florida, USA
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson, Micah C. Chambers and John D. van Horn (2013) Exploratory multimodal analysis of structural effects upon white matter due to intracranial hemorrhage Presentation at the Brain Injury Research Center, Ronald Reagan Medical Center, University of California, Los Angeles, May 7, 2013, Los Angeles, California, USA
- Andrei Irimia, Carinna M. Torgerson, Micah C. Chambers, Bo Wang, Marcel W. Prastawa, Guido Gerig, Ron Kikinis and John D. van Horn (2013) Beyond standard neuroimaging of the healthy brain: the challenge to develop robust image processing paradigms for the study of traumatic brain injury Invited Presentation at the Imaging Seminar of the Scientific Computing Institute, Department of Computer Science, University of Utah, April 27, 2013, Salt Lake City, Utah, USA
- John D. van Horn, Carinna M. Torgerson, Andrei Irimia, Micah C. Chambers, Jennifer S. Labus and Emeran A. Mayer (2013) Large scale brain networks Invited Presentation at the 11th Annual Central Nervous System Basic and Translational Science Symposium: “System Biological Approaches to Gut-Brain Interations in Health and Disease—From Molecular to Social Networks”, April 26, 2013 University of California, Los Angeles, California, USA
- John D. van Horn, Andrei Irimia, Micah C. Chambers and Ron Kikinis (2013) Modeling the network connectivity of a noted neurological case Invited Presentation, the Feinstein Institute for Medical Research, North Shore Jewish Hospital, March 20, 2013, Long Island, New York, USA
- John D. van Horn, Andrei Irimia, Micah C. Chambers and Ron Kikinis (2013) Mapping connectivity damage in a famous case of TBI Invited presentation, Department of Anatomical Sciences and Neurobiology, University of Louisville, January 24, 2013, Louisville, Kentucky,
- Andrei Irimia, Micah C. Chambers and John D. van Horn (2013) Research on brain connectomics and traumatic brain injury in the Laboratory of Neuro Imaging Presentation at the graduate student rotation meeting, Interdepartmental Neuroscience Program, January 16, 2013, University of California, Los Angeles, California, USA
- Anuja Sharma, Bo Wang, Andrei Irimia, Micah C. Chambers, John D. van Horn, Marcel W. Prastawa and Guido Gerig (2013) Four-dimensional diffusion tensor imaging analysis via longitudinal modeling of tract diffusivities Project activity presentation at the Ninth All Hands Meeting of the National Alliance for Medical Image Computing (NA-MIC), January 7-11, 2013, Marriott City Center Hotel, Salt Lake City, Utah, USA
- Bo Wang, Andrei Irimia, Micah C. Chambers, John D. van Horn, Marcel W. Prastawa and Guido Gerig (2013) Coregistration of structural and diffusion magnetic resonance imaging towards four-dimensional modeling of traumatic brain injury Project activity presentation at the Ninth All Hands Meeting of the National Alliance for Medical Image Computing (NA-MIC), January 7-11, 2013, Marriott City Center Hotel, Salt Lake City, Utah, USA
- Andrei Irimia, Bo Wang, Micah C. Chambers, John D. van Horn, Marcel W. Prastawa and Guido Gerig (2013) Clinically oriented structural, connectomic and functional analysis of traumatic brain injury in 3D Slicer Project activity presentation at the Ninth All Hands Meeting of the National Alliance for Medical Image Computing (NA-MIC), January 7-11, 2013, Marriott City Center Hotel, Salt Lake City, Utah, USA
- Andrei Irimia, Arthur W. Toga and John D. van Horn (2012) The study of brain connectivity using neuroimaging methodologies Invited research seminar presentation, A. T. Laurian National College, November 22, 2012, Botoşani, Romania
- Andrei Irimia, Sheng-Yang M. Goh, Carinna M. Torgerson and John D. van Horn (2012) Electroencephalographic modeling for source localization in traumatic brain injury via the finite element method Invited presentation at the Brain Injury Research Center, Ronald Reagan Medical Center, University of California, Los Angeles, November 13, 2012, Los Angeles, California, USA
- Andrei Irimia, Micah C. Chambers, Sheng-Yang Matthew Goh, Carinna M. Torgerson, Marcel W. Prastawa, Paul M. Vespa, David A. Hovda, Jeffry R. Alger, Guido Gerig, Stephen R. Aylward, Arthur W. Toga, Ron Kikinis and John D. van Horn (2012) Large scale calculation of the connectomic and network covariance of the human brain (N = 110) Poster Session of the National Alliance for Medical Image Computing, National Institute of Biomedical Imaging and Bioengineering, November 7-9, 2012, Bethesda, Maryland, USA
- Micah C. Chambers, Andrei Irimia, Lori L. Altshuler and John D. van Horn (2012) Structural and functional connectivity representation in euthymic bipolar disorder via connectogram representations Neuroscience Poster Session, Brain Research Institute, Ackerman Student Union Grand Ballroom, University of California, Los Angeles, December 4, 2012, Los Angeles, California, USA
- Andrei Irimia and John D. van Horn (2012) Multimodal neuroimaging for the personalized assessment of structural and connectomic brain changes prompted by traumatic brain injury Mazziotta Prize Presentation at the Work in Progress Meeting, Hermann Conference Center, Department of Neurology, University of California, Los Angeles, September 26, 2012, Los Angeles, California, USA
- Andrei Irimia, Micah C. Chambers and John D. van Horn (2012) Large-scale calculation of population-level connectomics using 3D Slicer and the connectogram. Presentation at “Big Data Computational Neuroscience using the Pipeline: LONI Resource Advisory Board Meeting”, Neurosciences Research Building Auditorium, Department of Neurology, University of California, Los Angeles, September 25, 2012, Los Angeles, California, USA
- Andrei Irimia, Micah C. Chambers, Bo Wang, Marcel W. Prastawa, Danielle F. Pace, Stephen R. Aylward, John D. van Horn, Guido Gerig (2012) Semi-automatic longitudinal segmentation of magnetic resonance imaging volumes in traumatic brain injury Invited Presentation at the Seventh Annual Project Week of the National Alliance for Medical Image Computing (NA-MIC), June 18-22, 2012, Greer Hall, Massachusetts Institute of Technology, Cambridge, Massachusetts, USA
- Andrei Irimia, Micah C. Chambers, Paul M. Vespa, David A. Hovda, Arthur W. Toga and John D. Van Horn (2012) Multimodal structural neuroimaging for patient-tailored longitudinal quantification of brain atrophy in traumatic brain injury Invited Presentation at the weekly Research Seminar of the Neural Dynamics and Data Analysis Laboratory, Department of Mathematics and Statistics, Boston University, June 15, 2012, Boston, Massachusetts, USA
- S. Y. Matthew Goh, Andrei Irimia, Paul M. Vespa and John D. van Horn (2012) Atlas-based automatic segmentation of MRI volumes from patients with traumatic brain injury Presentation at the Annual Science Day, University of California, Los Angeles, May 15, 2012, Los Angeles, California, USA
- Andrei Irimia, Micah C. Chambers, Paul M. Vespa, David A. Hovda, Arthur W. Toga and John D. Van Horn (2012) Connectomic visualization using the LONI Pipeline Invited Presentation at “Big Data Analysis using the LONI Pipeline” Advanced Neuroimaging, Informatics and Genomics Computing, Neurosciences Research Building Auditorium, Department of Neurology, University of California, Los Angeles, April 17, 2012, Los Angeles, California, USA
- Andrei Irimia, Micah C. Chambers and John D. van Horn (2012) The connectogram: a circular representation of human cortical networks Presentation at the Research Seminar of the Laboratory of Neuro Imaging, Department of Neurology, University of California, Los Angeles, February 9, 2012, Los Angeles, California, USA
- Bo Wang, Marcel W. Prastawa, Andrei Irimia, Micah C. Chambers, Paul M. Vespa, John D. van Horn and Guido Gerig (2012) Segmentation of longitudinal MR images of traumatic brain injury using a patient-specific framework Presentation at the Twenty-Fifth International Conference of SPIE—The International Society for Optical Engineering, February 4-9, 2012, San Diego, California, USA
- S. M. Matthew Goh, Andrei Irimia and John D. van Horn (2012) Semi-automatic segmentation and cortical mesh generation for traumatic brain injury MR volumes Presentation at the Fourth Annual Neurology Science Day, Department of Neurology, University of California, Los Angeles, January 25, 2012, Los Angeles, California, USA
- Micah C. Chambers, Andrei Irimia and John D. van Horn (2012) Full-brain functional connectivity using mutual information Presentation at the Fourth Annual Neurology Science Day, Department of Neurology, University of California, Los Angeles, January 25, 2012, Los Angeles, California, USA
- Andrei Irimia, SY Matthew Goh, Carinna M. Torgerson, Micah C. Chambers, Jeffry R. Alger, David A. Hovda, Paul M. Vespa, Arthur W. Toga, Ron Kikinis and John D. Van Horn (2012) Quantification of changes in cortical network topology caused by traumatic brain injury Presentation at the Fourth Annual Neurology Science Day, Department of Neurology, University of California, Los Angeles, January 25, 2012, Los Angeles, California, USA (the research outlined in this poster was awarded the Mazziotta Prize)
- John D. van Horn, Andrei Irimia and Micah C. Chambers (2012) Driving biological project on traumatic brain injury: an annual update Invited presentation at the Brain Injury Research Center, Ronald Reagan Medical Center, University of California, Los Angeles, January 17, 2012, Los Angeles, California, USA
- John D. van Horn, Andrei Irimia and Micah C. Chambers (2012) Traumatic brain injury Presentation at the Eighth All Hands Meeting of the National Alliance for Medical Image Computing, January 8-14, 2012, Salt Lake City, Utah, USA
- Andrei Irimia, Micah C. Chambers, Maria Filippou, Paul M. Vespa, Jeffry R. Alger, David A. Hovda, Arthur W. Toga, Ron Kikinis, John D. van Horn (2012) Impact of traumatic brain injury upon the architecture and longitudinal dynamics of cortical networks Presentation at the Thirtieth Dynamics Days 2012 International Conference on Chaos and Nonlinear Dynamics, January 4-7, 2012, Baltimore, Maryland, USA
- Marc Niethammer, Gabriel L. Hart, Danielle F. Pace, Micah C. Chambers, Andrei Irimia, John D. van Horn and Stephen R. Aylward (2011) Geometric metamorphosis for traumatic brain injury Presentation at the Fourteenth International Conference on Medical Image Computing and Computer-Assisted Intervention (MICCAI 2011), September 18-22, 2011, Toronto, Ontario, Canada
- Andrei Irimia, Micah C. Chambers, John D. van Horn (2011) Automatic segmentation of traumatic brain injury MRI volumes using atlas based classification and 3D Slicer Tutorial Presentation Session of the Seventh Annual Project Week of the National Alliance for Medical Image Computing, June 20-24, 2011, Massachusetts Institute of Technology, Cambridge, Massachusetts, USA
- Andrei Irimia, Micah C. Chambers, John D. van Horn (2011) Analysis and visualization of traumatic brain injury using 3D Slicer within the NA-MIC Collaboration Invited Presentation at the Seventh Annual Project Week of the National Alliance for Medical Image Computing, June 20-24, 2011, Massachusetts Institute of Technology, Cambridge, Massachusetts, USA
- Andrei Irimia, Micah C. Chambers, John D. van Horn (2011) Traumatic brain injury processing, analysis and visualization. Laboratory of Neuro Imaging, University of California, Los Angeles, June 3, 2011, Los Angeles, California, USA
- Andrei Irimia, John D. van Horn, Micah C. Chambers (2011) Longitudinal analysis of traumatic brain injury using 3D Slicer. Brain Injury Research Center, University of California, Los Angeles, March 25, 2011, Los Angeles, California, USA
- Andrei Irimia, John D. van Horn, Micah C. Chambers, Marcel W. Prastawa, Bo Wang, Silvain Gouttard, Paul M. Vespa, David A. Hovda, Jeffry R. Alger, Sonia M. A. Pujol, Guido Gerig, Stephen R. Aylward, Arthur W. Toga, Ron Kikinis (2011) Clinically-driven multimodal imaging of traumatic brain injury using semi-automatic segmentation in 3D Slicer. Third Annual Neurology Science Day, University of California, Los Angeles, January 26, 2011, Los Angeles, California, USA
- John D. van Horn, Andrei Irimia, Micah C. Chambers, Arthur W. Toga, Jeffry R. Alger, Paul M. Vespa, David A. Hovda (2011) UCLA Traumatic Brain Injury. Seventh All Hands Meeting of the National Alliance for Medical Image Computing (NA-MIC AHM), January 10-14 2011, Salt Lake City, Utah, USA
Press Releases
- Roberto Colon (2014) Simulando la lesion de las redes cerebrales [Simulating the lesion of brain networks] (in Spanish) http://robertocolom.blogspot.com/2014/03/simulando-la-lesion-de-las-redes.html
- Kurzweil (2014) First map of core white-matter connections of human brain developed at USC may help better address clinical challenges such as traumatic brain injury Kurzweilai.net
- Laura Sanders (2014) White matter scaffold offers new view of the brain: neural map may explain why some injuries are worse than others Science News: Magazine of the Society for Science and Public www.sciencenews.org
- Moj Doktor (2014) Socijalna mreža mozga [The social network of the brain] (in Croatian) http://www.mojdoktor.hr/article.php?id=4976&naziv=socijalna-mreza-mozga-
- Technologijos.lt (2014) Baltosios smegenų medžiagos jungčių žemėlapis: mūsų smegenys veikia kaip socialinis tinklas [White matter connections map: our brain works as a social network] (in Lithuanian) http://www.technologijos.lt/n/mokslas/zmogus_ir_medicina/S-38751/straipsnis/Baltosios-smegenu-medziagos-jungciu-zemelapis-musu-smegenys-veikia-kaip-socialinis-tinklas?l=2&p=1
- NeuroscienceNews.com (2014) Research reveals white matter ‘scaffold’ of human brain http://my-scientific-romance.tumblr.com/post/76394176275/neurosciencenews-research-reveals-white-matter
- Virtual Worldlets Network (2014) The human brain has a network backbone Virtualworldlets.net
- Ria Misra (2014) First map of your brain’s white matter helps understand brain injuries Ottersandsciencenews.blogspot.com
- Obekti.bg (2014) Това е първата карта, показваща всички връзки в бялото мозъчно вещество [This is the first map showing all connections in the white matter of the brain]
- Revfinlay.sld.cu (2014) Ciencia y technologia: revelan que la substancia blanca ejerce de “andamio” cerebral [Science and technology reveals that white matter serves as cerebral scaffold]
- tendencias21.net (2014) Explican por que pequenas lesions cerebrales pueden tener efectos devastadores [It is explained why small lesions can have devastating effects]
- Ben Thomas (2014) Brain-wide map of “neural highways” is first of its kind Scientific American Mind http://blogs.scientificamerican.com/mind-guest-blog/2014/02/20/brain-wide-map-of-neural-highways-is-first-of-its-kind/
- Claudio de Luca (2014) Cervello, le confessioni della material Bianca [The brain: revelations of the white matter] http://www.galileonet.it/articles/52fc8047a5717a1b16000027
- A Parrish (2014) Landmark map of brain’s white matter scaffold of network connections http://www.ineffableisland.com/2014/02/landmark-map-of-brains-white-matter.html
- F Pellizzari (2014) Rete del cervello: l’impalcatura della sostanza Bianca [Network of the brain: the scaffold of the white matter] http://www.alzheimer-riese.it/index.php?option=com_content &view=article&id=3595:rete-del-cervello-llimpalcaturar-della-sostanza-bianca&catid=36:ricerche& Itemid=233
- Ediciones Medicas (2014) Connectividad cerebral [Cerebral connectivity] http://www.ediciones medicas.com.ar/Actualidad/Ultimas_noticias/ Conectividad_cerebral
- Mokslo Lietuva (2014) Baltosios smegenu medziagos jungciu zemelapis http://mokslolietuva.lt/ 2014/02/baltosios-smegenu-medziagos-jungciu-zemelapis/
- Futurity.org (2014) ‘Scaffold’ map reveals brain’s weak spots http://www.futurity.org/brain-scaffold-map-pinpoints-vulnerable-spots/
- Ria Misra (2014) The first map showing all the connections in your brain’s white matter http://io9.com/the-first-map-showing-all-the-connections-in-your-brain-1520834855
Also covered by the following:
- Technobahn.com (2014) How our brain works: research reveals white matter ‘scaffold’ of human brain http://www.technobahn.com/articles/2014021115410031.html;
- Also covered by the following:
- http://medicalxpress.com/news/2014-02-brain-networks-reveals-white-scaffold.html;
- http://neurosciencestuff.tumblr.com/post/76348315832/how-our-brain-networks-research-reveals-white;
- http://elbiruniblogspotcom.blogspot.com/2014/02/frontiers-systematic-network-lesioning.html; http://neurosciencenews.com/white-matter-communications-network- neuroscience-746/; http://keatonaltom.tumblr.com/
- http://english.farsnews.com/newstext.aspx?nn=13921123000049
- http://news.asiacollege.ir/brain-networks-white-matter-scaffold-human-brain-revealed/
- Suzanne Wu (2014) Scientists create first map of brain ‘scaffold’ http://news.usc.edu/#!/article/58792/research-reveals-white-matter-scaffold-of-human-brain/
- solociencia.com (2013) Mas luz en torno al misterioso caso de Phineas Gage [More light shed on the mysterious case of Phineas Gage, in Spanish] Accessed March 12, 2013
- Vertical News Network (2012) Studies conducted at University of California on science recently published network.verticalnews.com May 21, 2012
- Stephanie S. O’Malley and Scott L. Rauch (2012) ACNP 2012 travel awardees American College of Neuropsychopharmacology www.acnp.org December 21, 2012
- Emily Elert (2012) The man who wasn’t there The Brain: a Discover Magazine Special, Fall 2012, pages 20-25
- Alexander Baklajian (2012) Human Connectome Project pieces together neural data through brain scans The Daily Bruin June 25, 2012
- Graziella Marturano (2012) Svelato il mistero di Phineas Gage [The mystery of Phineas Gage unveiled] (in Italian) Featured by Controcampus (Accessed May 30, 2012)
- Michael Robinson (2012) The 152-year-old brain that changed the course of science. Featured by The Market Oracle (Accessed May 29, 2012)
- British Psychological Society (2012) Neuroscience still haunted by Phineas Gage. Featured by Research Digest (Accessed May 23, 2012)
- Phineas Gage vivio 12 anos con una varilla en el cerebro [Phineas Gage lived for 12 years with a hole in his brain] (2012) Featured by Actualidad.com (Accessed May 22, 2012)
- Lauren Davis (2012) 164 years later, researchers map Phineas Gage’s pierced brain. Featured by io9 (Accessed May 20, 2012)
- Caroline Kraaijvanger (2012) Brein van onfortuinlijke Phineas Gage gereconstrueerd [Brain of unfortunate Phineas Gage reconstructed, in Dutch] Featured by Scientias.nl (Accessed May 21, 2012)
- Lancia gli trafigge la testa e cambia personalità. Svelato il «giallo medico» di Phineas Gage [A rod pierces his head and his personality changes. The ‘yellow doctor’ of Phineas Gage is unveiled, in Italian] (2012) Featured by Corriere della Sera (Accessed May 18, 2012)
- Без мозгов можно жить [You can live without a brain, in Russian] (2012) Featured by Siteua.org (Accessed May 18, 2012)
- Müfit Yılmaz Gökmen (2012) 164 yıllık mucizenin sırrı çözüldü [The secret of the miracle was solved after 164 years, in Turkish) Featured by MSNBC Turkey (Accessed May 17, 2012)
- David Freeman (2012) Phineas Gage brain map study spotlights neuroscience’s most celebrated case. Featured by The Huffington Post (Accessed May 18, 2012).
- Phineas Gage’s brain imaged for the first time (sic) (2012) Featured by Planetsave (Accessed May 17, 2012)
- Kyle Wagner (2012) Watch how a rod impaled a 19th century man’s skull without killing him Featured by Gizmodo (Accessed May 17, 2012)
- Clay Dillow (2012) Phineas Gage, neurology’s most interesting case, gets his head re-examined with new neural map Featured by Popular Science (Accessed May 17, 2012)
- Неврологи объяснили изменения психики Финеаса Гейджа после травмы головы [Neuroscientists explain Phineas Gage’s mental changes after head injury, in Russian] (2012) Med Portal (Accessed May 17, 2012)
- Lancia gli buca testa e diventa bad guy, svelato giallo del 1848 [Rod pierces his head and he becomes a bad guy, in Italian] (2012) Featured by Sassari Notizie (Accessed May 17, 2012)
- Omul care a uimit medicii timp de 200 de ani [The man who has astonished doctors for 200 (sic) years] (in Romanian) (2012) Realitatea (Accessed May 17, 2012)
- Kate Taylor (2012) Researchers map damage to Phineas gage’s brain. Featured by TG Daily, Free Republic, Science Blog (Accessed May 17, 2012)
- Helen Thomson (2012) Phineas Gage brain pathways mapped for the first time. Featured by New Scientist Health (Accessed May 17, 2012)
- Live Science Staff (2012) Phineas Gage’s missing brain mapped. Featured by Life Science (Accessed May 17, 2012)
- Robin Wulffson (2012) UCLA researchers study man with horrific brain injury. Featured by Examiner.com (Accessed May 16, 2012)
- Jacy Young (2012) Mapping Phineas Gage’s brain 150+ years later Featured by Advances in the History of Psychology (Accessed May 16, 2012)
- Lindsay Morton (2012) Modeling neurological damage of a traumatic brain injury survivor. Featured by EurekAlert!, Medical Xpress (Accessed May 16, 2012)
- Elizabeth Landau (2012) The curious brain impalement of Phineas Gage. Featured by CNN Health, Science Daily, Local 10, CNN Mexico (Accessed May 16, 2012)
- Thomas H. Maugh II (2012) Rod through Phineas Gage’s brain caused more damage than thought. Featured by Los Angeles Times (Accessed May 16, 2012)
- Mo Constandi (2012) Phineas Gage’s connectome Featured by The Guardian (Accessed on May 16, 2012)
- Mark Wheeler (2012) UCLA researchers map damaged connections in Phineas Gage’s brain. Featured by UCLA Newsroom, Science Codex, India Times, e! Science News, Newsodrome, SciTech Daily (Accessed on May 16, 2012)
- In Statu Nascendi (2012) Human brain becomes prettier 2012/02/human-brain-becomes-prettier.html February 9, 2012
- Circos (2012) Circos tackles the connectome [15] February 14, 2012
- Neuroskeptic (2012) Visualizing the connected brain http://neuroskeptic.blogspot.com February 8, 2012
- Michelle C. LaPlaca, David F. Meaney (2011) Perspectives on the role of bioengineering in neurotrauma research Journal of Neurotrauma volume 28, pages 2201-2202