Difference between revisions of "DBP2:Queens:PerkStation"
m |
m |
||
| Line 4: | Line 4: | ||
= PERK Station (Image overlay to perform/train image-guided needle interventions) = | = PERK Station (Image overlay to perform/train image-guided needle interventions) = | ||
| − | [[Image:CT-Image-Overlay-Zinreich.JPG| | + | [[Image:CT-Image-Overlay-Zinreich.JPG|450px|thumb|Image Overlay in clinical setup]] |
==Objective== | ==Objective== | ||
| Line 14: | Line 14: | ||
The PERK Station comprises of image overlay, laser overlay, and standard tracked freehand navigation in a single suite. The end-to-end solution software module along-with its hardware, operates in clinical environment. (To use training mode, developed for practical student instruction, use revision 5772.) | The PERK Station comprises of image overlay, laser overlay, and standard tracked freehand navigation in a single suite. The end-to-end solution software module along-with its hardware, operates in clinical environment. (To use training mode, developed for practical student instruction, use revision 5772.) | ||
| − | [[Image:Dani-PerkStation.JPG|thumb|320px|center|Perk Station in training / demo mode.]] | + | <!-- [[Image:Dani-PerkStation.JPG|thumb|320px|center|Perk Station in training / demo mode.]] --> |
| + | [[Image:Dani-PerkStation.JPG|thumb|320px|Perk Station in training / demo mode.]] | ||
The software enables to perform image-guided percutaneous needle biopsies. The workflow consists of four steps: | The software enables to perform image-guided percutaneous needle biopsies. The workflow consists of four steps: | ||
Revision as of 14:51, 6 April 2010
Home < DBP2:Queens:PerkStationBack to Queens DBP 2
PERK Station (Image overlay to perform/train image-guided needle interventions)
Objective
The objective of this project (PERK Station) is to develop a end-to-end solution implemented as a Slicer 3 module to assist in performing/training for image-guided percutaneous needle interventions. The software, along-with its hardware, overlays the image (CT/MR) acquired on the patient/phantom. The physician/trainee looks at the patient/phantom through a semi transparent mirror showing the image overlay and the CT/MR image appears to be floating inside the body with the correct size and position, as if the physician/trainee had 2D ‘X-ray vision’.
Description
The PERK Station comprises of image overlay, laser overlay, and standard tracked freehand navigation in a single suite. The end-to-end solution software module along-with its hardware, operates in clinical environment. (To use training mode, developed for practical student instruction, use revision 5772.)
The software enables to perform image-guided percutaneous needle biopsies. The workflow consists of four steps:
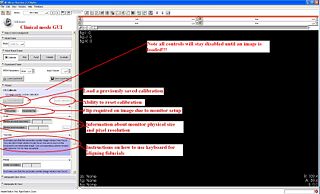
- Calibration:
- The objective of this step is to register the image overlay device with patient/phantom lying on scanner table. In this stage, the software sends the image to the secondary device, in correct physical dimensions. The secondary monitor is mounted with a semi-transparent mirror at 45 degree angle. Thus, the image displayed on monitor, gets projected on the mirror, and when seen through the mirror, the image appears to be floating on the patient/phantom. Based on how the secondary monitor is mounted w.r.t mirror, a horizontal or vertical flip may be required. Once correct flip arrangement in chosen, the image as seen on SLICER's slice viewer display should correspond to what is being seen through the mirror. Now the software enables the user who could be physician to translate/rotate the image as seen through the mirror, so that it aligns with the fiducials mounted/strapped on patient/phantom to achieve registration. This fiducial alignment achieves in-plane registration. For registration in z-plane, the image projection plane should be coincident with the laser-guide plane, which is also the plane of acquisition. It is worthwhile to mention that registration of image only takes place on the secondary monitor. Even though, the image is scaled, moved, rotated, and flipped, the image as displayed on the slice viewer of SLICER stays undisturbed. This enables the physician/user to zoom in/out of image in slice viewer for planning, without affecting the calibration. There is an option to save calibration done in a xml file, which is very useful.
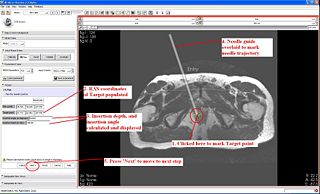
- Planning:
- Once the system is calibrated, and registered with patient, the software moves to next step. In this step, the entry and target points are given by mouse-clicks. The software calculates the insertion angle w.r.t vertical and insertion depth. Also, the software overlays the needle guide on the secondary monitor/mirror to assist the physician/user to perform the intervention. There is an option to reset the plan, in case the physician wishes to perform another needle intervention with same image.
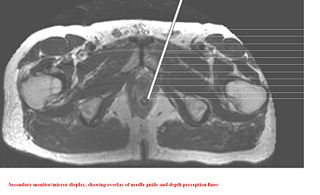
- Insertion:
- After planning, in the insertion step, further depth perception lines appear in gradations of 10mms to help the physician to insert the needle at correct depth.
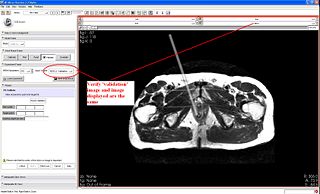
- Validation:
- After the needle insertion is complete, the physician/user acquires a validation image/volume with needle inside patient/phantom. The validation volume/image is added to scene. The physician/user can give the actual needle entry and end points to get error calculations.
Training mode: In training mode, it provides feedback to trainees in a controlled environment for performing image-guided percutaneous needle interventions. The workflow consists of an additional step of 'Evaluation' in addition to the four steps described earlier. In following description, only the difference are highlighted:
- Calibration:
- In this step, a different wizard GUI is loaded; the software does not automatically display the image in correct dimensions, rather it relies on the student/user's input. The calculation of amount of translation and rotation required to align the system is also left to the user.
- Planning:
- In this step too, the calculation of insertion depth and insertion angle is left to user to input.
- Insertion:
- This step is more or less the same
- Validation:
- This step is more or less the same
- Evaluation:
- In this step, various errors made in calculations are displayed to the student/user to objectively assess his/her performance in the intervention
Schedule
- 08/01/2009: Current status: All the core functionalities are implemented in a dynamically loadable Slicer module (one does not need to modify any of the Slicer code to use this module)
- 09/24/2009: Demonstration and tutorial: Demonstrated and provide one-on-one tutorials about the Perk Station on the MICCAI 2009 Conference (London, UK)
- 10/30/2009: Oblique slice support: Support needle insertion planning in any slice orientation.
- 11/30/2009: Software review: Review the software in terms of compliance to Slicer's interactive module architecture (with engineering core members).
Current deployment/usage:
- Clinical mode: The software has been delivered to team at Johns Hopkins University, Baltimore. It is currently being used in phantom and cadaver trials.
- Training mode: The software and hardware (designed and developed by Paweena U-Thainual and Iulian) integrated system has debuted as a part of Fall course at Queens' University in School of Computing for undergrad teaching taught by Dr Gabor Fichtinger.
Software source code:
Available on the NA-MIC Sandbox - access PerkStationModule
Tutorial
- Perk Station: PerkStationSlicerTutorial New
- Perk Station tutorial dataset: PerkStationTutorialDataset.zip New
- Perk Station hardware assembly instructions: coming soon...
Publications
- Vikal, S., P. U-Thainual, J. Carrino, I. Iordachita, G. Fischer, and G. Fichtinger, "Perk Station-Percutaneous surgery training and performance measurement platform", Computerized Medical Imaging and Graphics, June 2009.
- U-Thainual, P., G. Fischer, I. Iordachita, S. Vikal, and G. Fichtinger, "The Perk Station: Systems design for percutaneous intervention training suite", Procedings IEEE International Conference on Robotics and Biomimetics ROBIO 2009, pp. 1693–1697, 22–25 Feb, 2009.
- U-Thainual, P., I. Iordachita, S. Vikal, and G. Fichtinger, "Teaching Aid for Computer-Assisted Surgery", Eastern Ontario Symposium for Educational Technology, 2009.
- U-Thainual, P., I. Iordachita, and G. Fichtinger, "The Perk Station: Design of a percutaneous intervention training suite", 20th International Conference of the Society for Medical Innovation and Technology (SMIT), Vienna, Austria, August 28-31, pp. 148-153, 08/2008.
- Ahmidi, N., P. U-Thainual, S. Vikal, P. Mousavi, I. Iordachita, and G. Fichtinger, "A System for Performance Analysis of Surgeon Dexterity in Percutaneous Needle-based Interventions", 7th Imaging Symposium of the Imaging Network of Ontario, 2008.
- U-Thainual, P., G. Fischer, J. Carrino, G. Fichtinger, and I. Iordachita, "MR/CT Percutaneous Intervention Training Suite", 7th International Symposium on Interventional MRI, pp. 81-85, 2008.
- U-Thainual, P., S. Vikal, I. Iordachita, and G. Fichtinger, "The Perk Station: Portable training station for percutaneous interventions", Orthopaedic Care Conference, 2008.
Team
- PI: Gabor Fichtinger, Queen’s University (gabor at cs.queensu.ca)
- Hardware: Paweena U-Thainual, Queen's University(paweena at cs.queensu.ca), Iulian Iordachita, Johns Hopkins University (iordachita at jhu.edu)
- Software Engineer: Tamas Ungi (ungi at cs. queensu.ca), Andras Lasso (lasso at cs. queensu.ca), Siddharth Vikal, Queen’s University
- Queens Software Engineer Support: Csaba Csoma, Johns Hopkins University (csoma at jhu.edu)
- NA-MIC Engineering Contact: Katie Hayes, MSc, Brigham and Women's Hospital (hayes at bwh.harvard.edu)
- Host Institutes: Queen's University & Johns Hopkins University