DBP3:Utah:Reg Motiv
From NAMIC Wiki
Home < DBP3:Utah:Reg Motiv
Contents
Left Atrial Registration Image Types
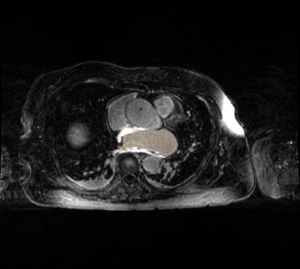
- The CARMA Center uses contrast-enhanced MRI images to evaluate new patients, predict procedural success, and evaluate therapeutic outcomes. The MRI images for each patient are further accompanied by MR angiographic images (MRA) and manual segmentations of relevant structures. These images are acquired longitudinally over the course of a patient's evaluation, treatment, and follow-up (i.e. months or years). Registration is often necessary to compare images from different time points in a patient's treatment, or even across patient cohorts at the same stage of disease progression or treatment.
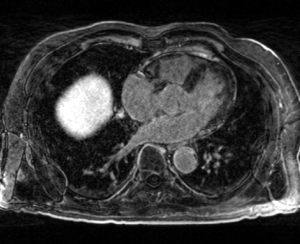
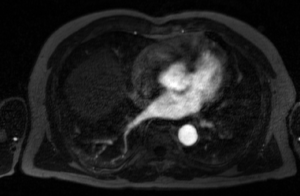
| Pre-ablation LGE-MRI Image | Post-ablation LGE-MRI Image |
|---|---|
| MRI image acquired approx. 15 minutes after contrast injection and prior to ablation. (The LA is the gray, horizontally oriented structure above the spine in the center of the image) | MRI image acquired approx. 15 minutes after contrast injection and after the ablation was performed. Sections of the LA wall which were ablated appear as hyper-enhanced pixels in the LA wall. |
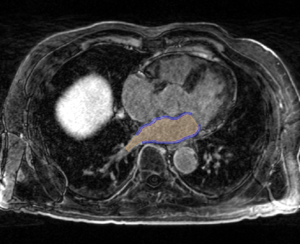
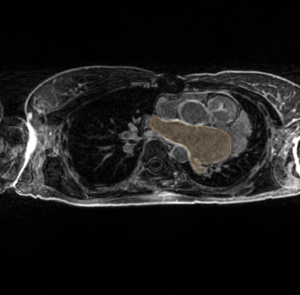
| MRA Image | Segmentation of LGE-MRI Image |
| The MRA is acquired after contrast injection and before the LGE-MRI images above. This image type highlights the blood pool of the LA and some surrounding structures. | Manual segmentation of the LA is performed on pre- and post-ablation LGE-MRI images by the CARMA team. Here the blue mask denotes the LA wall and the orange the blood pool. |
- The hallmark of atrial fibrillation is structural remodeling of the LA tissues. Changes to the LA myocardium are manifest as changes in the shape, composition, and thickness of the LA wall. Such changes can affect the accuracy of registration landmarks. In more extreme cases, the underlying anatomy can differ between patients, or even time points for the same patient, such that registration landmarks may appear or disappear from one case to the next.
- Common landmarks for image registration of the LA are the LA wall itself, the pulmonary veins, and the LA appendage.
LA Wall Abnormalities
- In addition to smaller, more common variations in LA shape, size, and wall thickness, there are some common disease states and procedurally-induced changes that affect registration of the LA. For example, some patients may have an abnormally large LA. Edema and non-enhanced regions in the LGE-MRI scans have also been observed that in some patients immediately after ablation therapy.
| Hypertrophic LA | Non-enhancing "no-reflow" LGE-MRI |
|---|---|
| Here the LA (blood pool delineated by the orange label mask) is quite a bit larger than normal; the left side (right side of the image) appears very dilated. | In this image the LA wall (region surrounding the blood pool -- orange label mask) has dark regions of non-enhancement. Large bright regions surround the LA wall tissue (possibly edema from the ablation procedure). |
Pulmonary Vein Anatomy
- The pulmonary veins (PVs) are important in the initiation and sustainment of AF, often harboring the electrical triggers responsible for AF. In an effort to remove or isolate these extraneous electrical signals, the PVs are often the target of ablation procedures; this often induces changes in the gross-anatomical structure of the PVs. The changes in PVs shape and structure caused by ablation make registration of the PVs non-trivial.
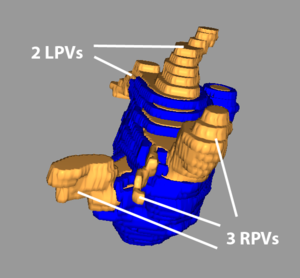
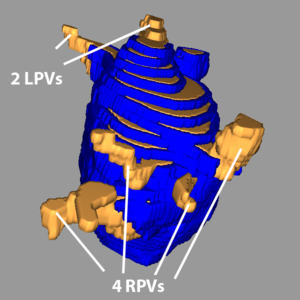
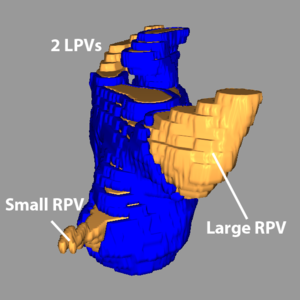
- The number of PVs across patients also differs; the typical configuration consists of 4 PVs: an inferior and superior vein on both the right and left sides of the LA. The most common deviations from this model are: a common left PV trunk, 3 right-side PVs, and 4 right-side PVs. Deviations in the number of PVs affects the landmarks used for image registration.
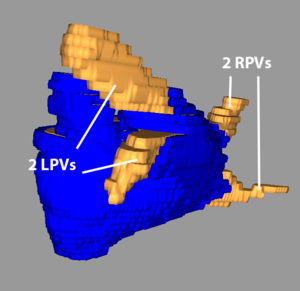
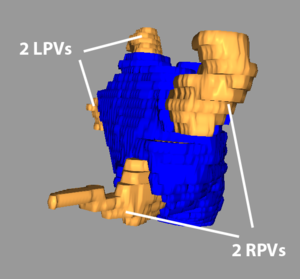
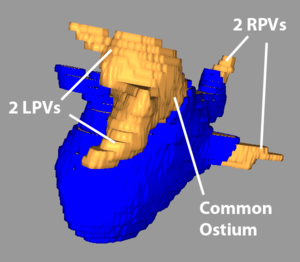
- Registration of the PVs has been approached using image-regsitration techniques rather than surface-registration techniques; the surfaces below are used because they show the variations in PV anatomy in a more clear and concise manner than the corresponding images.
| Typical LPVs | Typical RPVs |
|---|---|
| Normally, there are 2 distinct LPVs: one inferior and one superior. The superior vein tends to be larger than the inferior. (The blue volume represents the LA wall; the orange, the blood pool.) | Normally, there are 2 distinct RPVs: one inferior and one superior. These veins tend to be roughly the same size. |
| Common Left PV Ostium | 3 Right PVs |
| This LA has 2 LPVs; however, they share a common, larger-than-normal trunk. There are 2 normal RPVs. | This LA has 3 RPVs; the "middle" RPV is smaller than the other 2. There are 2 normal LPVs. |
| 4 Right PVs | Small and Large RPV |
| This LA has 4 RPVs; the "middle" 2 RPVs are smaller than the other 2. There are 2 normal LPVs. | Here, the number and placement of the veins is typical. However, the size of the 2 RPVs is atypical: one is larger and the other smaller than normal. |
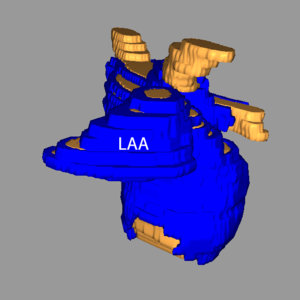
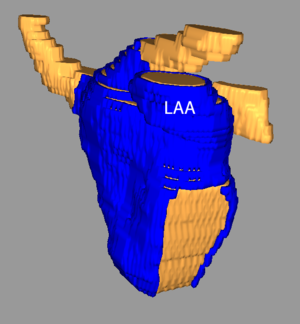
LA Appendage Variability
- The LA appendage is a muscular pouch connected to the upper, left portion of the LA. While the appendage doesn't aid in contraction, it is a common site for blood clot formation. The size, shape, and point of attachment of this region is also quite variable; this makes finding consistent registration landmarks in this region of the LA difficult.
| Typical LA Appendage | Small, Vertical LA Appendage |
|---|---|
| A "typical" LA appendage that extends out and then wraps back on the body of the LA. The appendage is denoted with "LAA". | A smaller and more vertical LA appendage than is typical. |
Conclusion
- In conclusion, registration of the LA is plagued by changes in various anatomical structures as the disease progresses and from one patient to the next.
- LA registration is further complicated by the thin LA walls and motion of the beating heart.