Project Week 25/Segmentation for improving image registration of preoperative MRI with intraoperative ultrasound images for neuro-navigation
Back to Projects List
Key Investigators
- Jennifer Nitsch (University of Bremen, Germany)
- Scheherazade Kraß (University of Bremen, Germany)
Project Description
| Objective | Approach and Plan | Progress and Next Steps |
|---|---|---|
|
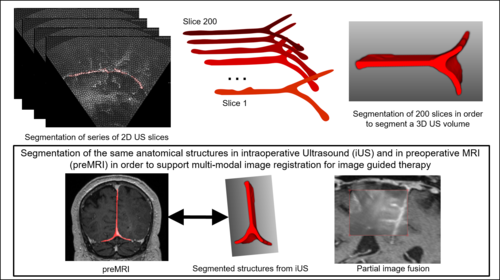
it would be to discuss in which "form" one or multiple segmented structures should influence the registration result. |
Illustrations
Using segmented structures as guiding frame for multi-modal image registration:
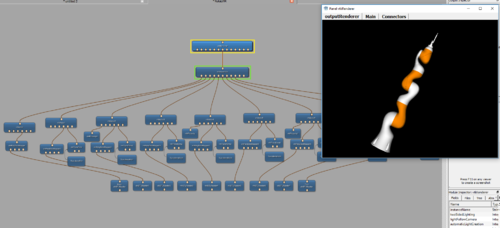
LWR Robot simulation in MeVisLab:
Background and References
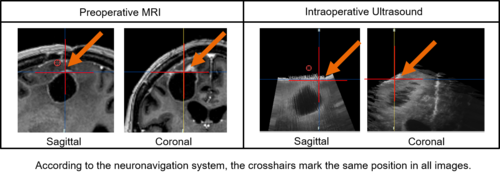
In glioma surgery neuronavigation systems assist in determining the tumor's location and estimating its extent. However, the intraoperative situation diverges seriously from the preoperative situation in the MRI scan displayed on the navigation system. The movement of brain tissue during surgery, i.e., caused by brainshift and tissue removal, must be considered mentally by the surgeon. A task that gets more challenging in later phases of the tumor resection.
Besides, it is an exhaustive issue and the shift of cerebral structures must be expected being non-uniform and that it implies a deformation of the image data. This makes it especially hard to mentally predict and model.
Thus, intraoperative imaging modalities are used to visualize the current intraoperative situation. IUS, for instance, is easy to use intraoperatively, offers real-time information, is widely available at low cost and causes no radiation. These are important advantages when iUS is compared with iCT or iMRI. However, in image-guided surgery precise image registration of iUS and preMRI and the thereon-based image fusion is still an unsolved problem. The different representations of cerebral structures in both modalities as well as artifacts within the iUS, hinder direct fusion of both modalities.