2010 Winter Project Week Musco Skeletal Segmentation
Key Investigators
- MIT: Michal Depa, Polina Golland
- BWH: Ehud Schmidt, Ron Kikinis
Objective
Atrial fibrillation is one of the most common heart conditions and can have very serious consequences such as stroke and heart failure. A technique called catheter radio-frequency (RF) ablation has recently emerged as a treatment. It involves burning the cardiac tissue that is responsible for the fibrillation. Even though this technique has been shown to work fairly well on atrial fibrillation patients, repeat procedures are often needed to fully correct the condition because surgeons lack the necessary tools to quickly evaluate the success of the procedure.
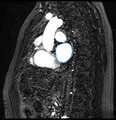
The objective of this project is to automatically segment the scar created by RF ablation in delayed enhancement MR images acquired after the procedure. We would then be able to present the surgeon with a visualization showing the size, shape and location of the scar.
Approach, Plan
Our earlier work focused on segmenting the left atrium (LA), the heart chamber on which RF ablations are usually done, in blood pool MR images. We used a label fusion segmentation algorithm which first registered all of the training images to the test one and then employed a weighted voting procedure at each voxel.
Given corresponding cardiac blood pool and post-procedure delayed enhancement images for each patient, our plan is to first segment the LA in the blood pool image, then transfer this segmentation to the delayed enhancement image of the same patient. We intend to use this prior information while searching for the ablation scar using intensity based algorithms. This prior knowledge of the LA location will allow us to avoid most false positives.
Progress
We have only done some very preliminary ablation scar segmentation experiments.