DBP3:MGH
Back to NA-MIC DBPs | NA-MIC Cores
Introduction
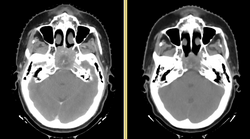
Head and neck cancers account for about 60,000 new cancer cases per year and represent about 6% of all cancers in the United States. These cancers are treated by a combination of chemotherapy, radiotherapy, and surgery. The five-year survival is approximately 50%. During a six-week regimen of radiotherapy, head and neck cancer patients often exhibit anatomic changes that affect their treatment. These changes include tumor regression or growth, changes in lymph node size, and changes in air cavities. Uncorrected, these changes can increase the risk of treatment complications or reduce treatment efficacy.
Adaptive radiotherapy is a form of personalized medicine that addresses the problem of anatomic change by incrementally adjusting the radiotherapy plan. However, a mid-treatment adjustment is complex: it requires a new CT image, image segmentation, deformable registration, and mapping of the previously delivered dose onto the new image. This project proposes to use the NA-MIC Kit to develop a simple, practical workflow for achieving adaptive radiotherapy which can be applied on a case-by-case basis.
For details on the background and goals, please see the project web page.
For a more extensive wishlist, see the planning meeting notes
Project Goals
This project has three specific aims:
- Develop an open computational workflow for adaptive radiotherapy.
- Validate the accuracy of image analysis algorithms for radiotherapy.
- Evaluate the dosimetric gain of adaptive radiotherapy.
External-beam radiotherapy requires a unique set of image analysis tools, which are only partly supported in the NA-MIC kit. Our specific aims require us to broaden the capabilities of 3D Slicer to support data interchange with commercial software, and to manipulate, review, and validate radiotherapy planning objects. We specify four sub-goals which we will work toward:
DICOM-RT Interchange
Structure and Dose Warping
Plan Review
Validation Tools
State of the Art: 2010
Research Plan
Key Personnel
- MGH: Greg Sharp, Annie Chan, George TY Chen, Nadya Shusharina, Rui Li, Ken Westover, Itai Pashtan, John Wolfgang
- MIT: Polina Golland, Michal Depa
- GT: Allen Tannenbaum, Ivan Kolesov
- Isomics: Steve Pieper