DBP3:MGH
Back to NA-MIC DBPs | NA-MIC Cores
Introduction
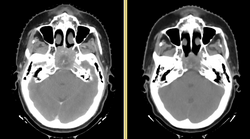
Head and neck cancers account for about 60,000 new cancer cases per year and represent about 6% of all cancers in the United States. These cancers are treated by a combination of chemotherapy, radiotherapy, and surgery. The five-year survival is approximately 50%. During a six-week regimen of radiotherapy, head and neck cancer patients often exhibit anatomic changes that affect their treatment. These changes include tumor regression or growth, changes in lymph node size, and changes in air cavities. Uncorrected, these changes can increase the risk of treatment complications or reduce treatment efficacy.
Adaptive radiotherapy is a form of personalized medicine that addresses the problem of anatomic change by incrementally adjusting the radiotherapy plan. However, a mid-treatment adjustment is complex: it requires a new CT image, image segmentation, deformable registration, and mapping of the previously delivered dose onto the new image. This project proposes to use the NA-MIC Kit to develop a simple, practical workflow for achieving adaptive radiotherapy which can be applied on a case-by-case basis.
Project Goals
This project has three specific aims:
- Develop an open computational workflow for adaptive radiotherapy.
- Validate the accuracy of image analysis algorithms for radiotherapy.
- Evaluate the dosimetric gain of adaptive radiotherapy.
External-beam radiotherapy requires a unique set of image analysis tools, which are only partly supported in the NA-MIC kit. Our specific aims require us to broaden the capabilities of 3D Slicer to support data interchange with commercial software, and to manipulate, review, and validate radiotherapy planning objects. We specify four sub-goals which we will work toward:
DICOM-RT Interchange
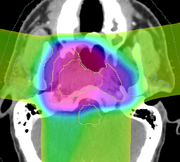
DICOM-RT is an open standard exchange format for radiotherapy objects. It is well established, and is supported by nearly every modern commercial software product. The DICOM-RT data set comprises four objects: RT Dose, RT Plan, RT Structure Set, and RT Image. Briefly, RT Plan specifies the treatment beams, including beam angles, beam sizes and apertures, couch angles, and radiation output. The RT Plan is associated with a CT image through the use of the DICOM UID mechanism. An RT Dose is the output of a dose computation, measured in Gray, and is similarly associated with both a CT image and an RT Plan. The RT Structure Set contains annotations of a CT image, either points or contours, and contains the geometric boundaries of organs and structures of interest. It is associated with a CT image. Finally, the RT Image is primarily used for 2D images used in patient positioning.
Our project goal for data interchange is to provide import and export capabilities for RT Dose and RT Structure Set in the NA-MIC kit. These two DICOM items form the minimal set necessary to implement adaptive radiotherapy. Import capabilities for RT Plan would also be useful as part of plan review, and we will implement this capability as time allows. RT Plan export and RT Image are outside of the scope of this project.
Structure and Dose Warping
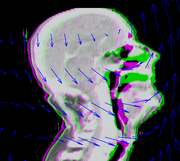
To quantify gains due to adaptive therapy, we will need to compare plans generated on pre-treatment CT scans with the same plans applied to mid-treatment scans. The scans will be matched using deformable image registration, and registration results will be used to warp structure sets and dose. Because only the pre-treatment scan contains structure sets, plan evaluation will require mapping structures from the pre-treatment to the mid-treatment scan. Similarly, to perform dosimetric comparisons requires mapping radiation dose.
While the NA-MIC kit contains a variety of algorithms, the workflow is not ideal for this application. Image registration in 3D Slicer creates deformed images, but we will require deformation maps that can be applied to the dose and structure sets. Our goal will be to improve the workflow to make it possible to re-use registration results for multiple subsequent operations.
Interactive Deformable Registration
Automatic deformable registration is the fastest and most convenient method for matching images, but there are cases where it gives sub-optimal results. In some cases, the results can be improved by adjusting the registration parameters, but in other cases the results do not improve.
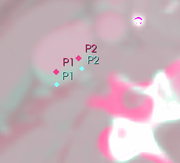
To guarantee that an acceptable registration can be achieved for all cases, we propose to develop interactive registration methods using point landmarks. We will focus on point landmarks because they are conceptually simple, and they are a good match with the fiducial tools already available in 3D Slicer. The operator can control the quality of the registration by choosing the number of landmarks and adjusting their locations.
Our goal is to provide tools that can generate registration results fully automatically, fully manually, or using a combined approach. In the combined approach, we will use automatic registration as the first stage of processing, and then the operator will adjust the results using the landmark registration method. To achieve this goal, we will need an additional tool for combining the two registration results.
Plan Review
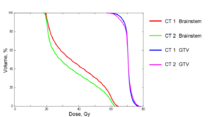
Evaluation of the dosimetry results will be performed using techniques that are well established in the radiotherapy field, such as isodose evaluation and dose volume histograms (DVHs). Although it would be possible to export images from 3D Slicer back into commercial systems to perform this analysis, it is a much better workflow to within the 3D Slicer. The goal of this project is therefore to provide sufficient capabilities within the 3D Slicer environment to perform plan review and comparison between nominal and adaptive plans. The minimum set of useful comparison tools to achieve this goal are isodose views, DVH generation, structure set manipulation, dose differencing, and gamma analysis.
Research Plan
Our research plan includes milestones for three years.
Year One
Year Two
Year Three
Links
Key Personnel
- MGH: Greg Sharp, Annie Chan, George TY Chen, Nadya Shusharina
- MIT: Polina Golland, Michal Depa
- GT: Allen Tannenbaum, Ivan Kolesov
- Isomics: Steve Pieper