Difference between revisions of "DBP3:UCLA"
Jack.vanhorn (talk | contribs) |
|||
| Line 57: | Line 57: | ||
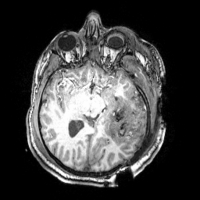
[[File:ThreeSubjects.png|200px|thumb|right|Sample images from the three TBI cases]]The following cases represent severe instances of TBI scanned using MRI brain imaging techniques. The (zipped) anatomical data files are in NIFTI format while DWI files are in Nrrd format. Additional data from PET and from CT will be forthcoming for these cases, as well. | [[File:ThreeSubjects.png|200px|thumb|right|Sample images from the three TBI cases]]The following cases represent severe instances of TBI scanned using MRI brain imaging techniques. The (zipped) anatomical data files are in NIFTI format while DWI files are in Nrrd format. Additional data from PET and from CT will be forthcoming for these cases, as well. | ||
| − | * [[ | + | * [[TBI Patient1 nrrd3.zip]] |
* [[File:TBI Patient2 nrrd2.zip]] | * [[File:TBI Patient2 nrrd2.zip]] | ||
* [[File:Patient3_DTI_nrrd_files.zip]] | * [[File:Patient3_DTI_nrrd_files.zip]] | ||
Revision as of 18:58, 5 January 2011
Home < DBP3:UCLABack to DBP Main
Contents
Introduction
What is traumatic brain injury?
Traumatic brain injury, often referred to as TBI, is most often an acute event that results in severe damage to portions of the brain. According to the CDC (United States Centers for Disease Control and Prevention), there are approximately 1.5 million people in the U.S. who suffer from a traumatic brain injury each year. 50,000 people die from TBI each year and 85,000 people suffer long term disabilities. In the U.S., more than 5.3 million people live with disabilities caused by TBI. Patients admitted to a hospital for TBI are included in this count, while those treated in an emergency room or doctor's office are not counted. The causes of TBI are diverse. The top three causes are: car accident, firearms and falls. Firearm injuries are often fatal: 9 out of 10 people die from such injuries. Young adults and the elderly are the age groups at highest risk for TBI. Along with a traumatic brain injury, persons are also susceptible to spinal cord injuries which is another type of traumatic injury that can result out of vehicle crashes, firearms and falls. Prevention of TBI is the best approach since there is no cure or way to reverse brain damage of this kind.
Mechanisms of TBI
Understanding the various mechanisms of TBI can be helpful for the development of robust and reliable computational algorithms for neuroimage data processing. These mechanisms are the highest causes of brain injury: Open head Injury, Closed Head Injury, Deceleration Injuries, Chemical/Toxic, Hypoxia, Tumors, Infections and Stroke.
1. Open Head Injury
* Results from bullet wounds, etc. * Largely focal damage * Penetration of the skull * Effects can be just as serious as closed brain injury
2. Closed Head Injury
* Resulting from a slip and fall, motor vehicle crashes, etc. * Focal damage and diffuse damage to axons * Effects tend to be broad (diffuse) * No penetration to the skull
3. Deceleration Injuries (Diffuse Axonal Injury) The skull is hard and inflexible while the brain is soft with the consistency of gelatin. The brain is encased inside the skull. During the movement of the skull through space (acceleration) and the rapid discontinuation of this action when the skull meets a stationary object (deceleration) causes the brain to move inside the skull. The brain moves at a different rate than the skull because it is soft. Different parts of the brain move at different speeds because of their relative lightness or heaviness. The differential movement of the skull and the brain when the head is struck results in direct brain injury, due to diffuse axonal shearing, contusion and brain swelling.
Diffuse axonal shearing: when the brain is slammed back and forth inside the skull it is alternately compressed and stretched because of the gelatinous consistency. The long, fragile axons of the neurons (single nerve cells in the brain and spinal cord) are also compressed and stretched. If the impact is strong enough, axons can be stretched until they are torn. This is called axonal shearing. When this happens, the neuron dies. After a severe brain injury, there is massive axonal shearing and neuron death.
4. Chemical/Toxic
* Also known as metabolic disorders * This occurs when harmful chemicals damage the neurons * Chemicals and toxins, e.g. insecticides, solvents, carbon monoxide poisoning, lead poisoning, etc.
5. Hypoxia (Lack of Oxygen)
* If the blood flow is depleted of oxygen, then irreversible brain injury can occur from anoxia (no oxygen) or hypoxia (reduced oxygen) * This condition may be caused by heart attacks, respiratory failure, drops in blood pressure and a low oxygen environment * This type of brain injury can result in severe cognitive and memory deficits
6. Tumors
* Tumors caused by cancer can grow on or over the brain * Tumors can cause brain injury by invading the spaces of the brain and causing direct damage * Damage can also result from pressure effects around an enlarged tumor * Surgical procedures to remove the tumor may also contribute to brain injury
7. Infections
* The brain and surrounding membranes are very prone to infections if the special blood-brain protective system is breached * Viruses and bacteria can cause serious and life-threatening diseases of the brain (encephalitis) and meninges (meningitis)
8. Stroke
* If blood flow is blocked through a cerebral vascular accident (stroke), cell death in the area deprived of blood will result * If there is bleeding in or over the brain (hemorrhage or hematoma) because of a tear in an artery or vein, loss of blood flow and injury to the brain tissue by the blood will also result in brain damage
In this DBP, we will be primarily concentrating on #'s 1, 2, and 3.
Example Neuroimaging Data Sets
The following cases represent severe instances of TBI scanned using MRI brain imaging techniques. The (zipped) anatomical data files are in NIFTI format while DWI files are in Nrrd format. Additional data from PET and from CT will be forthcoming for these cases, as well.
- TBI Patient1 nrrd3.zip
- File:TBI Patient2 nrrd2.zip
- File:Patient3 DTI nrrd files.zip
- File:Patient1 UCLA 3T.zip
- File:Patient2 UCLA 3T.zip
- File:Patient3 UCLA 3T.zip
- File:UCLA 1 5T.zip
- File:UCLA 3T.zip
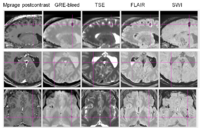
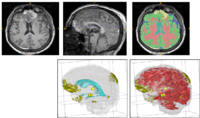
Example Results Obtained using Slicer
The following PDF contains a presentation prepared by Dr. Guido Gerig which showcases some example results on the above TBI data sets obtained using existing and newly developed Slicer processing modules.
Engineering Plans for the UCLA Driving Biological Project on Traumatic Brain Injury
The emphasis in this DBP is placed on the feasibility of subject-specific analysis, as opposed to population-based averaging, to examine the influence of TBI on time-dependent alteration of gray and white matter integrity with accompanying change in clinical outcome variables to be used in subsequent TBI assessment.
Specific Aims
This DBP [1] seeks to:
1. Develop end-to-end processing approaches using the NA-MIC Kit to investigate alterations in cortical thickness, and subsequent ventricular and white matter changes in patients with TBI and in age-matched controls. Image processing will include segmentation of lesions, hemorrhage, edema, and other pathology relevant to TBI. Longitudinal changes will be assessed by registration and joint segmentation of baseline and follow-up data.
2. Develop robust workflows for diffusion weighted imaging (e.g. DTI, HARDI) datasets from TBI patients, by using the NA-MIC Kit and Slicer to obtain reliable and robust metrics of white matter pathology and of white matter changes due to therapy and/or recovery.
3. Using the NA-MIC Kit, cross-correlate multimodal metrics of cortical thickness, complexity, ventricular volume, and lesions from structural imaging and white matter fiber integrity from diffusion tensor imaging, with clinical outcome variables, i.e., time since injury, age, gender and other potential factors predictive of recovery.
TBI Processing Requests
- multimodal registration within and between scan sessions (separated by ~6 months; what Sonia sketched out is on the right track)
- ABC segmentation (compiled for Windows!!)
- volume, surface, thickness, and other morphological metrics at time 1 and time 2
- changes in diffusion local to the lesions as well as overall mean FA and fiber patterns between scan sessions
- computation of "change" per unit time in each case
- visualization of the models and the degree of change
- generation of some sort of 'report' for each patient that the clinician can store and compare to changes in their neurological assessments. It would be nice if that report we not only PDF-like but also saved in some form of XML so that they could read it into Matlab, R, or some other secondary analysis framework or database without much trouble.
- Some of the segmentation may need to be user-guided but done so in a way that is easy for them to use. e.g. in order to conditionalize the segmentation given the presence of a lesion. Bleed, or other hypo(er)-intesity the user might point and click on the area in question, a boundary contour is found around that area, and the segmentation model is weighted by the presence of that area as some unique tissue type.
- creation of population-based atlases from multiple TBI subjects or at least reference to standardized coordinate systems
In Progress / Completed (Reverse Chronological)
- People are very interested in the ABC module but we understand that it has been difficult to compile for Windows (we all tend to be PC’s here with some exceptions)
- People have been curious about a macro capability to record selections for later playback
- People want semi-automated segmentation, etc
- Full brain fiber tractography
- NIFTI 4D file read/write, external gradient information importation, and a gradient table editor for DTI
- Better interoperability between LPS/RAS file organization in Slicer vs. vTK
- Ability to set direction cosines directly in Slicer volumes module
- Timed autosave functionality of scene files and other filetypes fundamental to Slicer (saved for several time steps)
- Welcome screen should be a pop-up window in the middle of screen that could be disabled
- Integration of volume render with slice displays (rendering set aside as an option)
- Import tools for DTIStudio and TrackVis tractography files
- Creating 3D ROIs using the edge detection routine
- Use of customizable toolbars for commonly used operations/features/modules/workflows/etc
- Volumes shouldn’t be loaded differently from “other data”
- Screen shot functionality shouldn’t force a re-render
- Being able to record video sequences (at least we couldn’t readily find this capability)
- NIFTI fMRI processing capability (3D+time)
Morphometric Processing
- Use of the ABC Module. Still needs compilation for Windows (64-bit) (Utah team)
DTI Processing
- TBD
Shape Analysis
- TBD
Data
- Need to obtain CT and PET for each example case (Jack Van Horn, UCLA TBI team)
Outreach
- TBI DBP Presentation at NA-MIC AHM (January 2011; Jack Van Horn)
- TBI Cases TBI Registration Case Library
- Develop comprehensive tutorial/how-to guide
- Design user friendly TBI workflow interface for Slicer
- Presentations/posters at OHBM, SFN, and other (inter)national meetings in year 2
- Hands-on teaching event for the DBP scientific community for year 3
- Peer reviewed publications
Investigators
- John Darrell Van Horn (UCLA) - DBP PI
- Andrei Irimia (UCLA)
- Micah Chambers (UCLA)
- Arthur W. Toga (UCLA)
- David Hovda (UCLA)
- Paul Vespa (UCLA)
- Jeffry Alger (UCLA)
- Guido Gerig (UTAH)
- Stephen Aylward (Kitware)
- Danielle Pace (Kitware)