Difference between revisions of "Projects:PathologyAnalysis"
| Line 55: | Line 55: | ||
[[File:Seg_algorithm_framework.png|600px|center|thumb|Segmentation framework]] | [[File:Seg_algorithm_framework.png|600px|center|thumb|Segmentation framework]] | ||
| + | |||
| + | === Construction of personalized atlas === | ||
| + | |||
| + | [[File:new1111.png|600px|center|thumb|Segmentation framework]] | ||
<center> | <center> | ||
Revision as of 04:49, 30 September 2011
Home < Projects:PathologyAnalysisBack to Utah 2 Algorithms
Analysis of Brain Images Presenting Variety of Cerebral Lesion Types
Description
Whereas methodologies for segmentation of normal anatomical structures and tissue types has become standard and highly automated, tools for efficient and reliable segmentation of pathology lag behind. Major efforts on segmentation of lesions mostly focus on wm lesions as in multiple sclerosis and tumor/edema segmentation.
Driven by challenging image analysis problems of the NA-MIC DBP partner UCLA on traumatic brain injury (TBI), we will develop image segmentation methodology that helps clinical researcher to characterize and quantify a variety of different cerebral lesion types. Standard automated image analysis methods are not robust with respect to the TBI-related changes in image contrast, changes in brain shape, cranial fractures, lesions, white matter fiber alterations, and other signatures of head injury.
We are working on an extension of the "atlas-based classification" method ABC for TBI datasets with the clinical goal to efficiently segment healthy brain tissue and cerebral lesions. A main goal will be the automated segmentation of healthy brain tissue and user-assisted segmentation of various cerebral lesion types (hematoma, subarachnoid hemorrhage, contusion and DAI, perifocal (regional) to diffuse (generalized) edema, hemorrhagic diffuse axonal injury (DAI)and more. A strong emphasis will be on the joint analysis of multiple imaging modalities (T1 pre- and T1 postcontrast, T2 (TSE), FLAIR, GRE, SWI, Perfusion, and DTI/DWI) for improved detection and quantitative characterization of lesion types.
Initial experiments
Experiments: Multi-modal registration and tissue segmentation
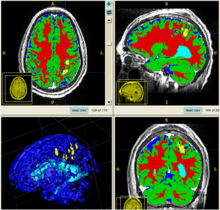
We conducted experiments with the application of the ABC tool to multi-modal image data of 5 TBI cases provided by DBP partner UCLA. The tool includes co-registration of multiple modalities via mutual-information linear registration, and a nonlinear registration (high-deformable fluid registration) of a probabilistic normative atlas for segmentation of healthy tissue. The following results show feasibility of multi-modal registration and segmentation of normal tissue. Pathology is segmented via postprocessing using 3D user-supervised level-set evolution.
Current work, jointly with the UCLA DBP partner, centers about a clinical definition of the most common lesion types and a multi-modality MRI characterization definition of these patterns. These characterizations will be used for the development of a segmentation methodology of the broad range of cerebral lesion types based on a user-guided definition of such patterns in current TBI cases.
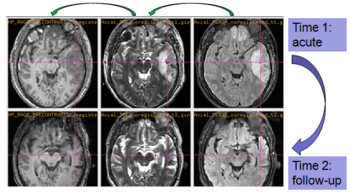
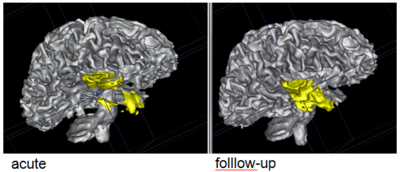
Experiments: Registration of longitudinal data
The NA-MIC DBP project on TBI analysis (UCLA partner) includes serial multi-modal MRI at acute phase and follow-up after six months. We test mutual-information-based linear registration of multi-modal MRI data within each time point and nonlinear registration (b-spline) of follow-up scans to obtain sets of images mapped into the same coordinate system. Preliminary results demonstrate the large deformations due to mass effect of a large lesion but also significant large regional changes of multi-modal MRI contrast from actute to follow-up.
Current progress (Sept. 2011)
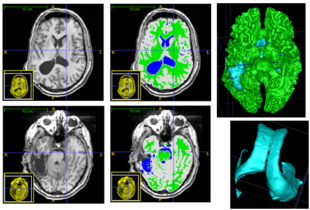
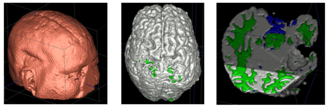
Patient-Specific Segmentation Framework for Longitudinal MR Images of Traumatic Brain Injury
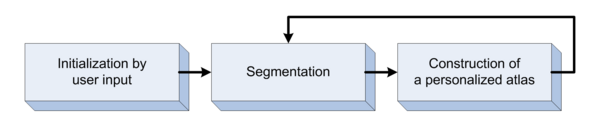
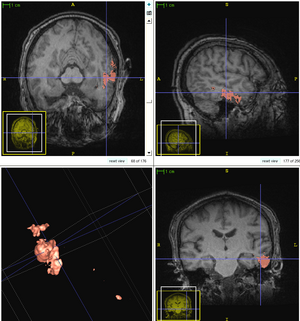
We propose a multi-modal image segmentation framework for longitudinal TBI images. The framework is initialized through manual input of primary lesion sites at each time point, which are then refined by a joint approach composed of Bayesian segmentation and construction of a personalized atlas. The personalized atlas construction estimates the average of the posteriors of the Bayesian segmentation at each time point and warps the average back to each time point to provide the updated priors for Bayesian segmentation. The difference between our approach and segmenting longitudinal images independently is that we use the information from all time points to improve the segmentations. Given a manual initialization, our framework automatically segments healthy structures (white matter, grey matter, cerebrospinal fluid) as well as different lesions such as hemorrhagic lesions and edema. Our framework can handle different sets of modalities at each time point, which provides flexibility in analyzing clinical scans.The segmentation of acute and chronic images using our framework are presented in the following figures. This work has been submitted to SPIE Medical Imaging 2012 [1].
Segmentation framework
The segmentation framework is initialized through manual input of primary lesion sites at each time point, which are then refined by a joint approach composed of Bayesian segmentation and construction of a personalized atlas. The following figure is the segmentation framework for multi-modal MR images.
Construction of personalized atlas
Collaboration events
(NA-MIC) all hands meeting (AHM) and Winter Project Week 2011
This is the first NA-MIC meeting between UCLA group and Utah group. During the project week, a lot of discussions have been done between the collaborators (UCLA and Utah groups) of this project. We worked together and answered each other's questions. Marcel introduced the purpose of all parameters of ABC and how these parameters would affect the final results. We discussed the possible user interaction we would use in the next step for better segmentation. Moreover, we knew more about the requirements of neurosurgeons and clinicians. Andrei pointed out the result of one subject was not good enough. Bo checked his results and redid the processing, and found the reason of the problem. Webpage of this event
(NA-MIC) Summer Project Week 2011
We prepared the preliminary algorithm for this project week. During the project week, we applied the preliminary algorithm to current data and fixed some bugs in the code. Our collaborators helped us to validate our current results of the supervised segmentation. We got some comments and feedback from our collaborators, which are very important for us to improve the current algorithm. Webpage of this event
Telephone meetings
Sept. 9th, 2011
During this telephone meeting, we discussed about the following problems.
- Integrate Mriwatcher to Slicer
- Manual segmentation and coregistration
- The SPIE submission
- The topological changes in TBI data
Conclusion
In this work, we will develop new methodologies and tools for user-guided segmentation of cerebral lesions in multi-modal brain MRI. Driving application is TBI imaging research as conducted by the NA-MIC DBP partner UCLA. Components to be included will be robust clustering as presented in [4], initialization of multi-modal intensity patterns via prior knowledge [4], and evaluation of generative models as presented in [2] and [3]. Developments will also include efficient user-guidance for localization and characterization of subject-specific lesion patterns, and tools to provide quantitative measurements and indices of spatial extent of pathologies currently used in clinical assessment. We will evaluate extension of the commonly used indices derived from 2D images to 3D shape features.
Literature
[1] Bo Wang, Marcel Prastawa, Andrei Irimia, Micah C. Chambers, Paul M. Vespa, John D. van Horn, Guido Gerig, A Patient-Specific Segmentation Framework for Longitudinal MR Images of Traumatic Brain Injury, SPIE Medical Imaging 2012. (submitted)
[2] Marcel Prastawa, Elizabeth Bullitt, Guido Gerig, Simulation of brain tumors in MR images, Medical Image Analysis 13 (2009), pp. 297-311, PMID: 19119055
[3] Marcel Prastawa and Guido Gerig, Brain Lesion Segmentation through Physical Model Estimation, International Symposium on Visual Computing ISVC 2008, LNCS, Vol. 5358, pp. 562--571.
[4] Marcel Prastawa, John H. Gilmore, Weili Lin, Guido Gerig, Automatic Segmentation of MR Images of the Developing Newborn Brain, Medical Image Analysis (MedIA). Vol 9, October 2005, pages 457-466
Key Investigators
- Utah: Bo Wang, Marcel Prastawa, Guido Gerig
- UCLA: John D. Van Horn, Andrei Irimia, Micah Chambers / Clinical partners: Paul Vespa, M.D., David Hovda, M.D.
References
Back to Utah 2 Algorithms